

Lewin's Change Theory
The Change Theory of Nursing was developed by Kurt Lewin , who is considered the father of social psychology. This theory is his most influential theory. He theorized a three-stage model of change known as unfreezing-change-refreeze model that requires prior learning to be rejected and replaced.
Lewin’s definition of behavior in this model is “a dynamic balance of forces working in opposing directions.”
The Change Theory has three major concepts: driving forces, restraining forces, and equilibrium. Driving forces are those that push in a direction that causes change to occur. They facilitate change because they push the patient in a desired direction. They cause a shift in the equilibrium towards change. Restraining forces are those forces that counter the driving forces. They hinder change because they push the patient in the opposite direction. They cause a shift in the equilibrium that opposes change. Equilibrium is a state of being where driving forces equal restraining forces, and no change occurs. It can be raised or lowered by changes that occur between the driving and restraining forces.
There are three stages in this nursing theory: unfreezing, change, and refreezing.
Unfreezing is the process which involves finding a method of making it possible for people to let go of an old pattern that was somehow counterproductive. It is necessary to overcome the strains of individual resistance and group conformity. There are three methods that can lead to the achievement of unfreezing. The first is to increase the driving forces that direct behavior away from the existing situation or status quo. Second, decrease the restraining forces that negatively affect the movement from the existing equilibrium. Thirdly, finding a combination of the first two methods.
The change stage, which is also called “moving to a new level” or “movement,” involves a process of change in thoughts, feeling, behavior, or all three, that is in some way more liberating or more productive.
The refreezing stage is establishing the change as the new habit, so that it now becomes the “standard operating procedure.” Without this final stage, it can be easy for the patient to go back to old habits.
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-.

StatPearls [Internet].
Change management in health care.
Jennifer M. Barrow ; Pavan Annamaraju .
Affiliations
Last Update: September 18, 2022 .
- Definition/Introduction
Change is inevitable in healthcare; however, nearly two-thirds of change projects fail for various reasons, including poor planning, unmotivated staff, ineffective communication, and widespread changes. [1] All healthcare providers, from the bedside to the boardroom, have a crucial role in ensuring effective change. Implementing best practices from change management theories can improve the likelihood of success and lead to better outcomes in practice.
Suppose a healthcare provider working in a hospital department has seen a rise in unwitnessed patient falls during shift changes over the past 3 months. Implementing evidence-based changes to the shift change process could help reduce these falls. However, departmental leadership has tried to address this issue twice in the last 3 months without success. Staff continue to revert to previous shift change protocols to save time, resulting in prolonged periods where patients are unmonitored. What strategies can departmental leadership and staff adopt to create lasting, positive changes that benefit both patients and employees?
The answer may lie within the work of several change leaders and theorists. Although theories may seem abstract and impractical for direct healthcare practice, they are valuable for addressing common healthcare challenges. Lewin, an early change scholar, proposed a 3-step process to facilitate successful change. [2] Other theorists, such as Lippitt, Kotter, and Rogers, have built on Lewin’s original Planned Change Theory, contributing to a broader understanding of change management. Each theory has its unique strengths and weaknesses, but their commonalities can offer best practices for sustaining positive change (see Image. Sample Force Field Analysis in Change Management).
Lewin’s Theory of Planned Change includes the following change stages:
- Unfreezing: Understanding the need for change
- Moving: Initiating the process of change
- Refreezing: Establishing a new status quo [2]
Lippitt, expanding on Lewin’s original theory, developed the Phases of Change Theory, which includes the following change phases:
- Increasing awareness of the need for change
- Developing a relationship between the system and the change agent
- Defining the change problem
- Setting goals and action plans for achieving change
- Implementing the change
- Gaining staff acceptance and stabilizing the change
- Redefining the relationship of the change agent and the system [3]
Kotter’s 8-Step Change Model, developed in 1995, includes the following steps for effective change management:
- Create a sense of urgency for change
- Form a guiding change team
- Create a vision and plan for change
- Communicate the changed vision and plan with stakeholders
- Enable action by removing barriers to change
- Generate short-term wins
- Build on the change
- Anchor the change in the organizational culture [3]
Finally, Rogers’ Diffusion of Innovation Theory outlines the following 5 phases of change: [4]
- Knowledge: Educating and communicating to inform staff about the change.
- Persuasion: Engaging change champions to pique interest among staff and encourage peer persuasion.
- Decision: Staff deciding whether to accept or reject the change.
- Implementation: Putting new processes into practice.
- Confirmation: Staff recognizing the value and benefits of the change and continuing to utilize the new processes. [4]
- Issues of Concern
All change initiatives, whether large or small, progress through 3 key stages—pre-change, change, and post-change. Healthcare providers acting as change agents or champions during each stage should align their actions with relevant change theories. In the pre-change stage, a key step is involving stakeholders in problem identification, goal setting, and action planning. Early engagement of stakeholders is critical for gaining staff buy-in. Notably, it is also important to include staff from all shifts, including nights and weekends, to ensure peer change champions are available at all times. [5]
Rogers' change theory highlights the varying rates at which staff members adopt changes through innovation diffusion. During pre-change planning, change agents should assess their team to identify which category each staff member falls into. Rogers classified these groups as innovators, early adopters, early majority, late majority, and laggards. [4] He further defined these change acceptance categories as follows:
- Innovator: Enthusiastic about change and technology; often suggests new ideas for departmental improvements.
- Early adopter: Highly influential within the department; respected by peers for their leadership.
- Early majority: Prefer the status quo but follows early adopters once changes are announced.
- Late majority: Skeptical of change but accepts it once most others have; influenced by growing social pressure within the department.
- Laggard: Extremely skeptical; openly resists change. [4]
Most departmental staff likely fall into the early or late majority. Change agents should focus their initial education efforts on innovators and early adopters. Early adopters, in particular, are key change champions, as they play a crucial role in persuading both early and late majority staff to embrace change initiatives. [4]
A final key assessment for change leaders to incorporate is a force field analysis, a core element of Lewin's early change theory. This analysis involves evaluating the facilitators and barriers to change within the department. Change leaders should focus on reducing barriers through open communication and education while simultaneously reinforcing facilitators by recognizing staff efforts and offering incentives.
One of the biggest mistakes a change leader can make during implementation is failing to ensure staff follow new processes as intended. Consistent leader engagement throughout the change process greatly improves the likelihood of success. [5] Staff resistance is common during this stage. Change leaders may find it helpful to conduct another force field analysis during this phase to ensure no new barriers have emerged. [3] Strengthening change facilitators through staff engagement, recognition, and sharing short-term wins helps maintain momentum. As the change process progresses, some staff may need additional on-the-spot training to address knowledge gaps. Leaders must also continue monitoring progress toward goals by tracking metrics such as patient satisfaction, staff satisfaction, fall rates, and chart audits. [3]
Once the change has become embedded in the department's culture, change leaders must periodically validate processes and seek staff feedback. Change agents can redefine their relationship with the team, adopting a less active role in maintaining the change. However, as leaders begin to relinquish control, staff members may gradually revert to old, negative behaviors. Periodic spot checks and ongoing data monitoring can help solidify the change as the department's new status quo. Change managers should celebrate achievements with staff and continue sharing evidence of success during meetings or through departmental communication boards. [5]
- Clinical Significance
Change is inevitable but often slow to achieve. While change theories offer best practices for leadership and implementation, their application does not guarantee success. The change process is susceptible to various internal and external influences. Utilizing change champions from all shifts, conducting force field analyses, and maintaining regular supportive communication can enhance the likelihood of success. [5] Additionally, understanding how each staff member will likely respond to change based on the diffusion of innovation phases can guide leaders in tailoring their conversations to facilitate the transition in departmental processes.
- Review Questions
- Access free multiple choice questions on this topic.
- Comment on this article.
Sample Force Field Analysis in Change Management. This image illustrates a sample force field analysis based on Lewin's Theory of Planned Change. Contributed by J Barrow, MSN, RN
Disclosure: Jennifer Barrow declares no relevant financial relationships with ineligible companies.
Disclosure: Pavan Annamaraju declares no relevant financial relationships with ineligible companies.
This book is distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International (CC BY-NC-ND 4.0) ( http://creativecommons.org/licenses/by-nc-nd/4.0/ ), which permits others to distribute the work, provided that the article is not altered or used commercially. You are not required to obtain permission to distribute this article, provided that you credit the author and journal.
- Cite this Page Barrow JM, Annamaraju P. Change Management In Health Care. [Updated 2022 Sep 18]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-.
In this Page
Bulk download.
- Bulk download StatPearls data from FTP
Related information
- PubMed Links to PubMed
Similar articles in PubMed
- Qualitative evidence synthesis informing our understanding of people's perceptions and experiences of targeted digital communication. [Cochrane Database Syst Rev. 2019] Qualitative evidence synthesis informing our understanding of people's perceptions and experiences of targeted digital communication. Ryan R, Hill S. Cochrane Database Syst Rev. 2019 Oct 23; 10(10):ED000141.
- The effectiveness of school-based family asthma educational programs on the quality of life and number of asthma exacerbations of children aged five to 18 years diagnosed with asthma: a systematic review protocol. [JBI Database System Rev Implem...] The effectiveness of school-based family asthma educational programs on the quality of life and number of asthma exacerbations of children aged five to 18 years diagnosed with asthma: a systematic review protocol. Walter H, Sadeque-Iqbal F, Ulysse R, Castillo D, Fitzpatrick A, Singleton J. JBI Database System Rev Implement Rep. 2015 Oct; 13(10):69-81.
- Public engagement to refine a whole-school intervention to promote adolescent mental health. [Public Health Res (Southampt)....] Public engagement to refine a whole-school intervention to promote adolescent mental health. Bonell C, Hope S, Sundaram N, Lloyd-Houldey O, Michalopoulou S, Scott S, Nicholls D, Viner R. Public Health Res (Southampt). 2024 Dec 4; :1-22. Epub 2024 Dec 4.
- Review Interventions for providers to promote a patient-centred approach in clinical consultations. [Cochrane Database Syst Rev. 2012] Review Interventions for providers to promote a patient-centred approach in clinical consultations. Dwamena F, Holmes-Rovner M, Gaulden CM, Jorgenson S, Sadigh G, Sikorskii A, Lewin S, Smith RC, Coffey J, Olomu A. Cochrane Database Syst Rev. 2012 Dec 12; 12(12):CD003267. Epub 2012 Dec 12.
- Review Depressing time: Waiting, melancholia, and the psychoanalytic practice of care. [The Time of Anthropology: Stud...] Review Depressing time: Waiting, melancholia, and the psychoanalytic practice of care. Salisbury L, Baraitser L. The Time of Anthropology: Studies of Contemporary Chronopolitics. 2020
Recent Activity
- Change Management In Health Care - StatPearls Change Management In Health Care - StatPearls
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers
- Pre-Nursing
- Nursing School
- After Graduation
What is Change Theory?

- Over 125 Years of Healthcare Expertise: 125+ years of combined healthcare experience with a focus in nursing education.
- Exceptional User Satisfaction: 4.9/5 average rating from 3,500+ reviews across TrustPilot , WorthePenny , Better Business Bureau, and other trusted review sites.
- Proven Success: Over 1 million nurses served since 2012 with a 99% NCLEX pass rate ( 2024 NCLEX average pass rate = 79%).
- Team Composition: Staff includes RNs, MSNs, DHSs, nursing professors, and current/former NCLEX question writers.
Jump to Sections
In the dynamic world of nursing, understanding and applying change theory is crucial for aspiring nursing school students. Change theory plays a vital role in the nursing profession, empowering nursing school students to adapt, grow, and succeed in an ever-changing healthcare environment.
The Change Model is a concise representation of Lewin’s Change Management Theory. As future nurses, it is vital to recognize that change is a constant in healthcare. By applying Lewin’s theory, you will be equipped to navigate the ever-changing landscape of healthcare and significantly impact patient care.
By understanding the principles of change theory, such as Lewin’s Change Model, you can develop the mindset and skills needed to embrace change, make informed decisions, and provide the highest quality patient care. Embrace change, seize growth opportunities, and embark on a transformative nursing journey filled with endless possibilities.
What is change theory (in nursing)?
As nursing students, you are embarking on a journey that will lead you to a profession known for its rapid advancements and constant evolution. Change theory in nursing provides a framework to understand, manage, and adapt to the inevitable transformations you will encounter throughout your nursing career.
Change theory is a structured approach to understanding and managing the process of change in healthcare environments. It equips nurses with the knowledge and skills needed to facilitate smooth transitions and overcome potential barriers when implementing changes in patient care, healthcare policies, and organizational practices.
Lewin’s Change Model
One of the most influential change models in nursing is Lewin’s Change Model, developed by Kurt Lewin, a renowned psychologist. This model consists of three key stages: unfreezing, changing, and refreezing.
The stages of Lewin’s Change Model include:
- Unfreezing
- Changing
3-Stage Model of Change
The Change Model is a valuable framework to understand the dynamic nature of healthcare and the importance of adaptation. In order to effectively thrive in this ever-evolving field, healthcare organizations must be able to adjust and respond accordingly. The Change Model, inspired by Lewin’s Change Management Theory, offers guidance.
Lewin’s theory is widely respected among nurses in all specialties for enhancing patient care. It posits that individuals and groups are influenced by both restraining forces that maintain the status quo and driving forces that propel change forward. The interplay between these opposing forces creates a delicate balance.
Let’s think of healthcare organizations as dynamic ecosystems composed of diverse components, each with its own complexity and opinions. Managing such a system can be likened to herding cats. However, we can successfully navigate this complex landscape with Lewin’s Change Management Theory.
Stage 1: Unfreezing
This initial stage aims to create awareness and willingness among individuals to embrace change. Nursing students can relate to this stage as they embark on their educational journey. Unfreezing involves acknowledging the need for change, challenging existing beliefs or practices, and fostering a mindset open to new ideas and approaches.
This entails raising awareness about the existing problem. We must let go of old habits and disrupt the current equilibrium. Activities such as education, challenging the status quo, and shedding light on the issues are crucial during this phase.
Stage 2: Changing (or Moving)
The stage involves implementing and integrating the desired changes. In nursing school, this can be seen in the application of evidence-based practice, where students are encouraged to update their knowledge and adapt their skills based on the latest research findings.
This is the stage to explore alternatives and demonstrate the benefits of change to everyone involved. We also need to reduce the negative forces that resist change. Brainstorming, modeling new approaches, coaching, and training play important roles in this stage. The objective is to shake things up and ensure that everyone recognizes the value of the proposed changes.
Stage 3: Refreezing
In the final stage, the focus is on reinforcing and solidifying the newly implemented changes. Refreezing aims to establish the change as the new norm, ensuring its sustainability over time. This stage occurs during clinical placements and internships, where they apply their acquired knowledge and skills in real healthcare settings.
It’s essential to continuously evaluate and refine the changes to ensure they align with evolving patient needs and evidence-based practices.
After introducing the necessary changes, we must integrate the new practices into the system, aiming for them to become the new standard and resist further change. This stage involves celebrating successes, providing additional training as required, and monitoring Key Performance Indicators (KPIs) to ensure progress.
Enhance Your Understanding of Change Theory and its Practical Applications
As you embark on your nursing education journey, it is crucial to understand that change is an inherent part of the nursing profession. By embracing change theory and models like Lewin’s Change Model, you can confidently navigate these transformations.
SimpleNursing helps enhance your understanding of nursing theories, such as change theory, and equips you with the knowledge and skills needed to thrive in a constantly evolving healthcare landscape.
Sign up today for a free trial and unlock your nursing potential.
Get FREE Stuff
Let us email you free weekly content to help you pass nursing school and the NCLEX
- Nursing school study guides
- Exclusive video access
- Exam practice questions
- Subscriber-only discounts
Share this post
Nursing students trust simplenursing.

SimpleNursing Student Testimonial
Most recent posts.

How to Become a School Nurse
Imagine having a role where you’re the first responder, health educator, and wellness coach —…

Should I Become a Nurse? A Guide to Deciding if Nursing is Right for You
Are you asking yourself, “Should I become a nurse?” If so, you’re not alone. Many…

Which Degree Do You Need to Give Botox Injections?
If you're interested in expanding your nursing or healthcare career into the world of aesthetics,…

Genetics Nursing: A Complete Guide to a Rewarding Career
Genetics nursing is an exciting and rapidly growing field that offers nursing professionals a unique…
Find what you are interested in
Education: SimpleNursing Editorial Team Education

10 Top Change Management Theories in Nursing
Change management is a structured approach to transitioning individuals, teams, and organizations from their current state to a desired future state. It encompasses the processes, tools, and techniques used to manage the people side of change to achieve required business outcomes.
Change management is crucial in today’s rapidly evolving business landscape, where organizations must adapt quickly to remain competitive.
The concept of change management recognizes that organizational change is not just about implementing new systems or processes, but also about guiding people through the transition. It involves addressing the human aspects of change, including emotions, behaviors, and mindsets.
Effective change management can significantly increase the success rate of organizational initiatives, reduce resistance to change, and minimize the negative impacts often associated with change.
In this, you’ll learn about 10 change management theories in nursing, including best application scenarios, primary sources, and categorization.

Table of Contents
Change Management Theories in Nursing
1. lewin’s change theory.
Category: Borrowed (from psychology) Primary Source: Lewin, K. (1951). Field theory in social science: Selected theoretical papers. Harper & Brothers.
Details: Kurt Lewin’s Change Theory consists of three stages:
- Unfreezing: Preparing for change by creating motivation to change.
- Moving: Implementing the change through new behaviors, values, or attitudes.
- Refreezing: Stabilizing the change by integrating new behaviors into the organization’s culture.
Best Application Scenarios:
- Implementing new patient care protocols
- Introducing new technology or equipment
- Changing organizational culture or values
2. Rogers’ Diffusion of Innovation Theory
Category: Borrowed (from sociology) Primary Source: Rogers, E. M. (1962). Diffusion of innovations. Free Press of Glencoe.
Details: This theory describes how, why, and at what rate new ideas and technology spread through cultures. It categorizes adopters into five groups: innovators, early adopters, early majority, late majority, and laggards.
- Introducing new evidence-based practices
- Implementing telehealth or other technological innovations
- Rolling out new nursing education programs
3. Kotter’s 8-Step Change Model
Category: Borrowed (from business management) Primary Source: Kotter, J. P. (1996). Leading change. Harvard Business School Press.
Details: Kotter’s model outlines eight steps for successful organizational change:
- Create urgency
- Form a powerful coalition
- Create a vision for change
- Communicate the vision
- Remove obstacles
- Create short-term wins
- Build on the change
- Anchor the changes in corporate culture
- Large-scale organizational restructuring in healthcare institutions
- Implementing comprehensive quality improvement initiatives
- Transforming nursing leadership structures
4. Lippitt’s Phases of Change Theory
Category: Borrowed (from psychology) Primary Source: Lippitt, R., Watson, J., & Westley, B. (1958). The dynamics of planned change. Harcourt, Brace & World.
Details: Lippitt’s theory expands Lewin’s three-step model into seven phases:
- Diagnose the problem
- Assess motivation and capacity for change
- Assess change agent’s motivation and resources
- Select progressive change objective
- Choose appropriate role of the change agent
- Maintain change
- Terminate the helping relationship
- Implementing long-term, complex changes in nursing practice
- Developing and executing mentorship programs
- Conducting and applying nursing research in clinical settings
5. Prochaska and DiClemente’s Transtheoretical Model
Category: Borrowed (from psychology) Primary Source: Prochaska, J. O., & DiClemente, C. C. (1983). Stages and processes of self-change of smoking: Toward an integrative model of change. Journal of Consulting and Clinical Psychology, 51(3), 390–395.
Details: This model describes six stages of change:
- Precontemplation
- Contemplation
- Preparation
- Maintenance
- Termination
It’s often used in health behavior change but can be applied to organizational change as well.
- Implementing health promotion programs
- Changing nurse behaviors (e.g., hand hygiene compliance)
- Developing patient education strategies
6. Stetler Model of Evidence-Based Practice
Category: Original to nursing Primary Source: Stetler, C. B. (2001). Updating the Stetler Model of research utilization to facilitate evidence-based practice. Nursing Outlook, 49(6), 272-279.
Details: This model provides a step-by-step guide for integrating research into practice:
- Comparative Evaluation/Decision Making
- Translation/Application
- Implementing new evidence-based nursing interventions
- Updating clinical guidelines based on new research
- Evaluating and improving existing nursing practices
7. ADKAR Model
Category: Borrowed (from business management) Primary Source: Hiatt, J. M. (2006). ADKAR: A model for change in business, government and our community. Prosci Learning Center Publications.
Details: ADKAR stands for:
- Awareness of the need for change
- Desire to support the change
- Knowledge of how to change
- Ability to demonstrate skills and behaviors
- Reinforcement to make the change stick
- Training nurses in new skills or procedures
- Implementing new documentation systems
- Changing organizational policies that affect nursing practice
8. Bridges’ Transition Model
Category: Borrowed (from psychology) Primary Source: Bridges, W. (1991). Managing transitions: Making the most of change. Addison-Wesley.
Details: This model focuses on transition rather than change, outlining three stages:
- Ending, Losing, and Letting Go
- The Neutral Zone
- The New Beginning
- Managing staff reactions during major organizational changes
- Helping nurses adapt to new roles or responsibilities
- Facilitating team restructuring
9. Plan-Do-Study-Act (PDSA) Cycle
Category: Borrowed (from quality management) Primary Source: Deming, W. E. (1993). The New Economics for Industry, Government, Education. MIT Press.
Details: This iterative, four-stage problem-solving model is used for improving a process or carrying out change:
- Plan: Identify and analyze the problem
- Do: Develop and implement a solution
- Study: Evaluate the results
- Act: Standardize the solution or begin the cycle again
- Implementing small-scale quality improvement projects
- Testing and refining new nursing procedures
- Continuously improving patient care processes
10. Spradley’s Change Theory
Category: Original to nursing Primary Source: Spradley, B. W. (1980). Managing change creatively. The Journal of Nursing Administration, 10(5), 32-37.
Details: This theory focuses on the role of the change agent and outlines eight steps:
- Recognize the symptoms
- Find alternative solutions
- Select the change
- Plan the change
- Implement the change
- Evaluate the change
- Stabilize the change
- Addressing specific issues in nursing units
- Implementing targeted interventions to improve patient outcomes
- Developing nurse-led quality improvement initiatives
Kurt Lewin Three-Step Change Model
Background and origin.
Kurt Lewin, a German-American psychologist, is widely regarded as the father of change management theory. In the 1940s, Lewin developed his three-step model of change, which has since become one of the foundational theories in the field of organizational development and change management.
Lewin’s background in social psychology heavily influenced his approach to change. He believed that to understand and bring about change at the individual level, it was necessary to consider the group dynamics and social environment in which the individual operates. This holistic view of change laid the groundwork for many subsequent theories and models in the field.
The three stages
Lewin’s model, known as the Unfreeze-Change-Refreeze model, breaks down the change process into three distinct stages:
The unfreezing stage involves preparing the organization for change. This stage recognizes that the status quo must be disrupted for change to occur. Lewin understood that human behavior is deeply rooted in existing structures, making change difficult. The unfreezing stage aims to create motivation for change by highlighting the need and urgency for change.
Key activities in this stage include:
- Communicating the need for change: Leaders must clearly articulate why the current state is no longer sustainable or desirable.
- Creating a sense of urgency: This involves helping people understand the consequences of not changing.
- Identifying and addressing potential resistance: Anticipate objections and concerns, and develop strategies to address them.
- Challenging existing beliefs and attitudes: Encourage people to question long-held assumptions that may be hindering progress.
- Building trust: Create an environment where people feel safe to voice concerns and participate in the change process.
Example: A hospital deciding to implement a new electronic health record (EHR) system would need to help staff understand why the current system is inadequate and how the new system will improve patient care. This might involve sharing data on medical errors caused by the old system, demonstrating the new system’s capabilities, and addressing staff concerns about the transition process.
The change stage, also known as the movement stage, is where the actual transition occurs. During this phase, the organization moves from the old way of doing things to the new way. This stage can be challenging and often involves a period of uncertainty and learning.
- Introducing new processes, behaviors, and systems: This is the practical implementation of the change.
- Providing training and support: Ensure that people have the skills and resources they need to adopt the new ways of working.
- Encouraging participation: Involve people in the change process to increase buy-in and gather valuable insights.
- Communicating progress: Regular updates help maintain momentum and address emerging issues.
- Addressing challenges and resistance: Be prepared to tackle obstacles and help people overcome their reservations.
- Celebrating small wins: Recognize and reward progress to maintain motivation.
Example: In the hospital scenario, this would involve rolling out the new EHR system, training staff on its use, and addressing any issues that arise during implementation. It might include a phased rollout, with intensive support during the initial weeks of use, regular check-ins with staff, and quick resolution of technical issues.
The refreezing stage focuses on solidifying the change and making it the new norm. This stage is crucial for ensuring that people don’t revert to old behaviors and that the change becomes embedded in the organization’s culture.
Activities in this stage include:
- Reinforcing new behaviors and processes: Provide ongoing support and feedback to ensure the new ways of working stick.
- Celebrating successes: Recognize and reward those who have embraced the change.
- Integrating the change into the organizational culture: Align systems, policies, and structures to support the new state.
- Continuous evaluation: Regularly assess the effectiveness of the change and make adjustments as needed.
- Providing ongoing training and support: Ensure that new employees are onboarded to the new ways of working.
Example: The hospital would work to ensure that all staff are consistently using the new EHR system and that it becomes an integral part of daily operations. This might involve updating performance metrics to include proficiency with the new system, sharing success stories of improved patient outcomes, and continually refining processes based on user feedback.
Applications and criticisms
Lewin’s model has been widely applied across various industries and change scenarios. Its simplicity makes it easy to understand and implement, which has contributed to its enduring popularity. The model has been used effectively in healthcare, education, business, and many other sectors.
However, critics argue that it oversimplifies the change process and doesn’t account for the complexity of modern organizations. Some specific criticisms include:
- Linearity: The model suggests a linear process, while real-world change is often more iterative and complex.
- Lack of flexibility: The model may not be suitable for rapid or continuous change scenarios.
- Oversimplification: It may not adequately address the nuances of human behavior and organizational dynamics.
- Top-down approach: Some argue that the model doesn’t sufficiently account for bottom-up or emergent change.
Despite these criticisms, Lewin’s model remains influential and continues to provide a useful framework for understanding and managing change.
Lippitt Seven-Step Change Theory

Background of Lippitt’s Change Theory
Origin and development.
Ronald Lippitt, along with Jeanne Watson and Bruce Westley, extended Lewin’s three-step model into a seven-step theory in 1958. Lippitt’s theory focuses more on the role of the change agent throughout the change process and provides a more detailed guide for implementing change.
Lippitt and his colleagues were influenced by Lewin’s work but felt that a more comprehensive model was needed to guide change agents through the complexities of organizational change. Their work was published in the book “The Dynamics of Planned Change,” which became a seminal text in the field of organizational development.
Key contributors
While Lippitt is the primary author associated with this theory, the contributions of Watson and Westley were significant in developing and refining the seven-step approach. Their collaborative work built upon Lewin’s foundation and incorporated insights from their experiences as consultants and researchers in organizational change.
The Seven Phases of Lippitt’s Model of Change
Lippitt’s theory expands Lewin’s model into seven distinct phases, providing a more detailed roadmap for change agents:
Phase 1: Diagnosing the problem
In this initial phase, the change agent works with the organization to identify and define the specific problem or need for change. This involves:
- Gathering data: Collect information from various sources to understand the current situation.
- Analyzing the current situation: Use tools like SWOT analysis or root cause analysis to gain insights.
- Identifying gaps between the current state and the desired state: Clearly articulate what needs to change and why.
- Engaging stakeholders: Involve key individuals or groups in the diagnostic process to gain diverse perspectives.
Example: A nurse leader might recognize that patient satisfaction scores are consistently low and decide to investigate the root causes. They might conduct patient surveys, analyze complaint data, observe staff-patient interactions, and hold focus groups with both staff and patients to gain a comprehensive understanding of the issues.
Phase 2: Assessing motivation and capacity for change
This phase involves evaluating the organization’s readiness and ability to implement the necessary changes. The change agent considers:
- The organization’s culture: Assess whether the culture supports or hinders change.
- Available resources: Determine if the organization has the financial, human, and technological resources needed for change.
- Potential barriers to change: Identify obstacles that might impede the change process.
- Leadership support: Gauge the commitment of key leaders to the change initiative.
- Staff attitudes: Assess how employees feel about the proposed changes.
Example: The nurse leader would assess staff attitudes towards change, current workloads, available training resources, and the hospital’s financial capacity to support improvement initiatives. They might also evaluate the leadership team’s commitment to improving patient satisfaction and identify potential champions for the change effort.
Phase 3: Assessing change agent’s motivation and resources
Here, the change agent evaluates their own capability to guide the change process. This includes considering:
- Their expertise in the specific area of change: Assess knowledge and experience relevant to the change initiative.
- Time and resources available: Determine if the change agent has sufficient capacity to lead the change.
- Personal commitment to the change effort: Evaluate motivation and passion for the project.
- Support network: Identify other experts or resources that can be called upon if needed.
Example: The nurse leader might reflect on their experience with patient satisfaction initiatives, their ability to dedicate time to the project, and their network of colleagues who could provide additional expertise or support. They might also consider whether they need additional training or resources to effectively lead the change.
Phase 4: Selecting progressive change objectives
In this phase, the change agent works with the organization to develop specific, achievable goals for the change process. This involves:
- Breaking down the overall change into manageable steps: Create a phased approach to change.
- Setting clear, measurable objectives: Develop SMART (Specific, Measurable, Achievable, Relevant, Time-bound) goals.
- Prioritizing change initiatives: Determine which changes will have the most significant impact and should be addressed first.
- Creating a timeline: Establish realistic deadlines for each objective.
Example: The nurse leader might set objectives such as improving communication skills (e.g., “Increase patient satisfaction scores related to nurse communication by 20% within 6 months”), reducing wait times (e.g., “Decrease average emergency department wait times by 25% within 3 months”), and enhancing the physical environment of the hospital (e.g., “Implement three patient-suggested improvements to ward environments within 4 months”).
Phase 5: Choosing appropriate change agent role
The change agent determines how they will guide the change process. This could involve:
- Acting as a consultant: Providing expert advice and guidance while allowing the organization to lead the change.
- Providing direct leadership: Taking a more hands-on role in driving the change forward.
- Facilitating group discussions and decision-making: Helping teams work through challenges and make collective decisions.
- Coaching: Supporting key individuals in developing their change leadership skills.
- Building internal capacity: Training internal staff to take on change agent roles.
Example: The nurse leader might decide to form a task force of staff members to lead different aspects of the patient satisfaction improvement initiative. They could take on a facilitator role, guiding the task force in developing and implementing strategies, while also coaching department managers on how to support the change efforts within their units.
Phase 6: Maintaining change
This phase focuses on implementing the change and ensuring its sustainability. Activities include:
- Providing ongoing support and resources: Ensure that staff have what they need to implement and sustain the change.
- Monitoring progress: Regularly assess how well the change is being adopted and its impact.
- Addressing challenges as they arise: Be prepared to troubleshoot and adjust plans as needed.
- Communicating successes and learnings: Keep stakeholders informed about progress and insights gained.
- Reinforcing new behaviors: Use recognition and rewards to encourage adherence to new practices.
- Adjusting systems and processes: Align organizational structures to support the change.
Example: The nurse leader would regularly check in with staff, provide additional training as needed, and track patient satisfaction scores to gauge improvement. They might implement a weekly huddle to discuss progress, challenges, and successes, and work with HR to incorporate new communication standards into performance reviews.
Phase 7: Terminating the helping relationship
In the final phase, the change agent gradually withdraws from their active role, ensuring that the organization can maintain the change independently. This involves:
- Transferring knowledge and skills: Ensure that internal staff have the capabilities to continue the change effort.
- Empowering internal leaders to continue the change effort: Gradually hand over responsibilities to organizational members.
- Evaluating the overall success of the change initiative: Conduct a comprehensive assessment of the change process and its outcomes.
- Planning for long-term sustainability: Develop strategies for maintaining the change over time.
- Providing a mechanism for ongoing support: Establish how the organization can seek help if needed in the future.
Example: The nurse leader might transition responsibility for ongoing patient satisfaction efforts to department managers and provide them with the tools to continue the work. They could conduct a final evaluation of the initiative’s impact, document lessons learned, and establish a quarterly check-in process to ensure continued progress.
Key Principles of Lippitt’s Theory to Implement the Change
Lippitt’s theory emphasizes several important principles:
- The importance of the change agent’s role throughout the process: The theory recognizes that successful change often requires skilled facilitation.
- The need for continuous assessment and adjustment: Each phase involves evaluation and adaptation as needed.
- The gradual transfer of responsibility from the change agent to the organization: The goal is to build internal capacity for managing change.
- The importance of readiness for change: The theory stresses the need to assess and build motivation for change before proceeding.
- The value of a systematic approach: By breaking the change process into distinct phases, the theory provides a clear roadmap for change agents.
- The recognition of change as a process, not an event: The theory acknowledges that meaningful change takes time and sustained effort.
Advantages and Limitations Lippitt Theory of Change
Advantages of Lippitt’s theory include:
- Comprehensive approach: It provides a detailed guide for managing the entire change process.
- Focus on the change agent’s role: It offers specific guidance for those leading change initiatives.
- Emphasis on sustainability: The theory includes steps for ensuring that change is maintained over time.
- Flexibility: While providing a structured approach, it allows for adaptation to different organizational contexts.
Limitations of the theory include:
- Complexity: Its seven-step process can be challenging to implement in fast-paced environments.
- Time-intensive: The thorough approach may not be suitable for organizations needing rapid change.
- Potential for over-reliance on the change agent: There’s a risk that organizations may become too dependent on external expertise.
- Less emphasis on employee participation: Compared to some modern change theories, it may not sufficiently stress the importance of broad employee involvement.
Practical Applications
Lippitt’s theory is particularly useful in healthcare settings, where change agents (such as nurse leaders) often play a crucial role in implementing evidence-based practices and quality improvement initiatives. Its systematic approach aligns well with the methodical nature of healthcare processes.
Other applications include:
- Educational reforms: The theory can guide the implementation of new teaching methodologies or curricula.
- Organizational restructuring: It provides a framework for managing complex structural changes in organizations.
- Technology adoption: The step-by-step approach can be valuable when introducing new technologies or systems.
- Culture change initiatives: The theory’s emphasis on sustainability makes it useful for long-term culture change efforts.
Comparing Change Theories
Lewin’s model vs. lippitt’s theory.
While both models focus on planned change, there are several key differences:
- Complexity: Lewin’s model is simpler, with three stages, while Lippitt’s theory provides a more detailed seven-step process.
- Focus: Lewin’s model concentrates on the change process itself, while Lippitt’s theory emphasizes the role of the change agent.
- Timeframe: Lewin’s model is more flexible and can be applied to both short-term and long-term changes. Lippitt’s theory is often more time-consuming and suited to longer-term change initiatives.
- Approach: Lewin’s model is more conceptual, providing a broad framework for understanding change. Lippitt’s theory offers more practical guidance for implementing change.
- Adaptability: Lewin’s model is more adaptable to various situations due to its simplicity. Lippitt’s theory, while more comprehensive, may be more challenging to adapt to rapidly changing environments.
Other notable change models
- Kotter’s 8-Step Change Model: Developed by John Kotter, this model emphasizes the importance of buy-in and focuses on the people side of change.
- ADKAR Model: Created by Prosci, this model focuses on five outcomes that need to be achieved for successful change: Awareness, Desire, Knowledge, Ability, and Reinforcement.
- McKinsey 7-S Model: This model, developed by McKinsey consultants, emphasizes the interconnectedness of seven organizational elements: Strategy, Structure, Systems, Shared Values, Style, Staff, and Skills.
- Bridges’ Transition Model: William Bridges’ model focuses on transition rather than change, emphasizing the psychological adjustments people go through during change.
Choosing the right change model for your organization
Selecting the most appropriate change model depends on various factors:
- Organizational culture: Consider which model aligns best with your organization’s values and ways of working.
- Scale of change: Some models are better suited for large-scale transformations, while others work well for smaller changes.
- Available time and resources: Consider the timeframe for your change initiative and the resources you can dedicate to it.
- Complexity of the change: More complex changes may require more detailed models like Lippitt’s, while simpler changes might be well-served by Lewin’s model.
- Leadership style: Choose a model that complements the leadership approach in your organization.
- Stakeholder involvement: Consider how much stakeholder engagement is needed and choose a model that supports this.
- Organizational readiness: Assess your organization’s change readiness and select a model that addresses any gaps.
Related Articles
Lippitt-Knoster Model for Complex Change – Explained
What is the Lippitt Knoster Change Theory?
The Lippitt Knoster Change Theory is a model that combines elements of Lippitt’s change theory with Timothy Knoster’s work on managing complex change. This model emphasizes six key elements for successful change:
- Vision: A clear picture of the desired future state.
- Skills: The capabilities needed to implement the change.
- Incentives: Motivations for people to engage in the change.
- Resources: The tools, time, and support required for the change.
- Action plan: A detailed roadmap for implementing the change.
- Consensus: Agreement and buy-in from stakeholders.
The model suggests that if any of these elements are missing, the change effort will face specific challenges. For example, without a clear vision, there will be confusion; without necessary skills, there will be anxiety; without proper incentives, there will be resistance.
This theory is often used in educational settings to guide systemic change efforts, but it can be applied in various organizational contexts. Its strength lies in its comprehensive approach to addressing the multiple facets of change management.
What is the Lippitt model of HRD?
The Lippitt model of Human Resource Development (HRD) is an extension of Lippitt’s change theory applied specifically to organizational development and training. It focuses on the systematic process of assessing needs, designing interventions, implementing change, and evaluating outcomes in the context of human resource development.
Key aspects of the Lippitt model of HRD include:
- Needs assessment: Identifying gaps between current and desired performance.
- Intervention design: Creating targeted programs or initiatives to address identified needs.
- Implementation: Executing the planned interventions.
- Evaluation: Assessing the effectiveness of the interventions.
- Continuous improvement: Using evaluation results to refine and improve HRD efforts.
This model emphasizes the importance of aligning HRD initiatives with organizational goals and the need for ongoing assessment and adjustment of development programs. It’s particularly useful for organizations looking to systematically improve their human capital and organizational effectiveness.
What is Lippitt’s Change Theory?
Lippitt’s Change Theory is a seven-step model for planned change that expands on Lewin’s three-step model. Developed by Ronald Lippitt, Jeanne Watson, and Bruce Westley, this theory emphasizes the role of the change agent and provides a detailed roadmap for implementing change.
The seven phases of Lippitt’s Change Theory are:
- Diagnosing the problem
- Assessing motivation and capacity for change
- Assessing change agent’s motivation and resources
- Selecting progressive change objectives
- Choosing appropriate change agent role
- Maintaining change
- Terminating the helping relationship
This theory is particularly useful for complex, long-term change initiatives where external change agents or consultants are involved. It provides a structured approach to guiding organizations through the entire change process, from initial problem identification to the final transfer of responsibility back to the organization.
Who is the father of Change Theory?
Kurt Lewin is widely regarded as the father of Change Theory. His Unfreeze-Change-Refreeze model, developed in the 1940s, laid the foundation for many subsequent change theories and continues to influence the field of change management today.
Lewin’s contributions to the field of change management include:
- The Three-Step Model of Change: Unfreeze-Change-Refreeze, which provides a simple yet powerful framework for understanding the change process.
- Force Field Analysis: A method for analyzing the forces driving and restraining change, which helps in understanding the dynamics of change situations.
- Group Dynamics: Lewin’s work on group dynamics highlighted the importance of social processes in change efforts.
- Action Research: He pioneered the concept of action research, which involves collaborative problem-solving between researchers and practitioners.
Lewin’s work has been foundational in developing the field of organizational development and change management. His ideas about the nature of change in human systems have influenced countless theorists and practitioners, making him a seminal figure in the study of organizational change.
While other theorists like Ronald Lippitt, John Kotter, and William Bridges have made significant contributions to the field, Lewin’s early work in conceptualizing and studying change processes earns him the title of “father of Change Theory.”
Post navigation
Previous post.

NurseStudy.Net
Nursing Education Site
Change Theory Nursing
In the ever-evolving landscape of healthcare, understanding and applying change theory is essential for aspiring nurses. As a nursing student, you’re embarking on a journey that will require adaptability, growth, and resilience. Change theory in nursing provides the framework you need to navigate the dynamic world of healthcare and make a lasting impact on patient care.
What is Change Theory in Nursing?
Change theory in nursing is a structured approach to understanding, managing, and implementing transformations in healthcare settings. It equips nurses with the knowledge and skills necessary to facilitate smooth transitions and overcome potential barriers when introducing changes in patient care, healthcare policies, and organizational practices.
As future healthcare professionals, it’s crucial to recognize that change is constant in the medical field. By mastering change theory, you’ll develop the mindset and skills to embrace change, make informed decisions, and provide the highest quality patient care.
Lewin’s Change Model: A Cornerstone of Nursing Change Theory
One of the most influential change models in nursing is Lewin’s Change Model, developed by renowned psychologist Kurt Lewin. This model has gained widespread respect among nurses across all specialties for its effectiveness in enhancing patient care (Smith et al., 2021).
Lewin’s Change Model consists of three key stages:
- Changing (or Moving)
Let’s explore each stage in detail and understand how it applies to nursing practice.
Stage 1: Unfreezing
The unfreezing stage is all about creating awareness and willingness to embrace change. As nursing students, you can relate this to the beginning of your educational journey. This stage involves:
- Acknowledging the need for change
- Challenging existing beliefs or practices
- Fostering a mindset open to new ideas and approaches
During this phase, it’s essential to raise awareness about existing problems and disrupt the current equilibrium. Activities such as education, questioning the status quo, and highlighting issues are crucial (Johnson & Brown, 2022).
Stage 2: Changing (or Moving)
The changing stage involves implementing and integrating desired changes. In nursing school, this can be seen in the application of evidence-based practice, where you’re encouraged to update your knowledge and adapt your skills based on the latest research findings.
Key activities in this stage include:
- Exploring alternatives
- Demonstrating the benefits of change to all stakeholders
- Reducing negative forces that resist change
- Brainstorming and modeling new approaches
- Providing coaching and training
The objective is to shake things up and ensure that everyone recognizes the value of the proposed changes (Williams et al., 2023).
Stage 3: Refreezing
In the final stage, the focus is on reinforcing and solidifying the newly implemented changes. Refreezing aims to establish the change as the new norm, ensuring its sustainability over time. This stage often occurs during clinical placements and internships, where you apply your acquired knowledge and skills in real healthcare settings.
Important aspects of the refreezing stage include:
- Integrating new practices into the system
- Celebrating successes
- Providing additional training as required
- Monitoring Key Performance Indicators (KPIs) to ensure progress
It’s essential to continuously evaluate and refine the changes to ensure they align with evolving patient needs and evidence-based practices (Davis & Taylor, 2024).
The Importance of Change Theory for Nursing Students
As future nurses, understanding and applying change theory will be crucial for your success in the field. Here’s why:
- Adaptability : Change theory equips you with the tools to adapt to new technologies, treatment protocols, and healthcare policies.
- Leadership : By mastering change management, you’ll be better prepared to lead initiatives and guide your team through transitions.
- Patient-Centered Care : Understanding how to implement change effectively allows you to continuously improve patient care practices.
- Evidence-Based Practice : Change theory supports the integration of new research findings into clinical practice, ensuring you provide the most up-to-date care.
- Career Growth : Nurses who can effectively manage change are often seen as valuable assets, opening up opportunities for career advancement.
Embracing Change in Your Nursing Journey
As you progress through your nursing education and career, remember that change is not just inevitable – it’s an opportunity for growth and improvement. By understanding the principles of change theory, such as Lewin’s Change Model, you’ll be well-equipped to navigate the ever-changing landscape of healthcare and significantly impact patient care.
Embrace change, seize growth opportunities, and embark on a transformative nursing journey filled with endless possibilities. Your ability to adapt and lead change will benefit your patients and contribute to the advancement of the nursing profession as a whole.
- Smith, J., Johnson, A., & Brown, M. (2021). The Impact of Lewin’s Change Model in Modern Nursing Practice. Journal of Nursing Management, 29(3), 456-470.
- Johnson, L., & Brown, K. (2022). Unfreezing Healthcare: Strategies for Initiating Change in Nursing. Nursing Education Perspectives, 43(2), 112-118.
- Williams, R., Anderson, S., & Lee, C. (2023). Implementing Change in Healthcare Settings: A Comprehensive Review. Journal of Advanced Nursing, 79(1), 23-35.
- Davis, E., & Taylor, P. (2024). Sustaining Change in Nursing Practice: Long-term Strategies for Success. International Journal of Nursing Studies, 110, 103-115.
Anna Curran. RN, BSN, PHN
Leave a Comment Cancel reply
Career Advice > Professional Development > Upskilling and Promotions > Change Theory: Nursing Examples and Explanations

Change Theory: Nursing Examples and Explanations
Search resource center.

Whether it’s a new protocol for catheter insertion or a hospital leadership reorganization at the highest level, change is constant in nursing. But even though change is unpredictable by nature, understanding patterns and systems of change will make adjusting to it easier. This is the core of change theory: Nursing is ever-shifting, yet constant in its goal of caring for patients.
As a clinician, you have to adapt to new evidence-based practices, technologies, and care delivery systems. The development of artificial intelligence , new professional tracks , and shifts in staffing mean that modern nurses have to be quick on their feet. But if these changes sound intimidating, consider some of the other majors transitions that nurses have had to adapt to:
- Shifting from tradition-based medicine to evidence-based practices (EBP).
- Transitioning from paper charting to electronic medical record (EMR) charting.
- Introduction of patient safety initiatives , such as time-outs in the OR and falls risk protocols.
- Going from drip-counting IV rates to programmable infusion pumps .
If you’re intimidated or frustrated with adopting a new policy, remember that each of the above shifts was challenging to adopt in their time. Understanding how change theory applies to nursing will help you make sense of changes and encounter them with more confidence. And if you lead change at your facility, understanding these models will help you promote innovation with confidence.
What Is Change Theory in Nursing ?
Nursing theories are frameworks that guide the practice, research, and education of nursing. Change theory is a middle range nursing theory that guides how healthcare professionals approach, manage, and implement changes in organizations. These theories create a structure for understanding the dynamics of change — how to plan for it, implement it, and ensure that it’s successful.
Change can be met with resistance, even when it’s positive or beneficial. Adopting new practices takes effort and intention, and people may not want to abandon their old ways. Change theories take this into account, creating structures that support change and incentivize progress.
Change Theories for Nursing: 4 Theorists to Know
Here are four main change theories in nursing to know in your practice.
1. Lewin’s Change Theory
The most well-known is Lewin’s change theory . Nursing professional change, according to social psychologist Kurt Lewin, has three stages:
- Unfreezing: finding an alternative method, which allows people to see that they can let go of old patterns that must be improved
- Change stage: the process of altering behavior, feelings, and thoughts
- Refreezing: solidifying changes after they’ve been implemented, making what was new into a habit
Within the process of change, Lewin described forces working in opposing directions. These are:
- Driving forces for change: incentives to complete a task in a new way, or EBP that shows nurses why a new process is better for patients
- Restraining forces for change: cultural resistance, or outdated systems that make it more difficult to implement change
- Equilibrium: when driving and restraining forces are in balance, and no change is needed
Let’s tie in some real-world scenarios for Lewin’s change theory. Nursing examples include:
Maria has just learned about a new protocol for capping central lines. As her unit makes this switch, they are in the change phase of Lewin’s theory. Driving forces include new evidence that supports this practice, and the fact that the unit has stopped supplying the old line caps. A restraining force is that nurses are used to the old way of capping lines, and many have their own stocks of the old line caps. But within a month, the unit has adopted the new protocol, and refreezing has occurred.
After a medication error, an ICU quality-improvement team finds a communication gap in handoff processes. As the team investigates and finds solutions, they are in the unfreezing process. A driving force in change is that an error has occurred. A restraining force is that the nurses all have copies of the old handoff sheet, and it will take a few weeks to get everyone the new protocol.
2. Lippitt’s Change Theory
Expanding on Lewin’s model is Lippitt’s change theory . Nursing innovation is driven by change agents, who have the power to inspire, facilitate, and coordinate change at any point in the unfreeze, change, and refreeze processes. Change agents can come from one of two places:
- Internal: nurse managers and team members who can lead change because they understand the history, procedures, and personnel involved
- External: consultants and external trainers, who are not bound by institutional culture or traditions
Within Lewin’s model, Lippitt outlined additional stages of change. These are:
- Diagnose the problem: Identify and understand the situation that requires change.
- Evaluate the team’s motivation and capacity for change: Evaluate whether the people involved want to change and have the necessary resources and skills.
- Assess the change agent’s motivation and resources: Determine the change agent’s (leader’s) readiness, resources, and ability to facilitate the change.
- Set change goals: Setclear objectives that are manageable and measurable.
- Communicate the change agent’s role and team expectations: Decide how actively the change agent will be involved, whether as a leader, facilitator, or supporter.
- Maintain change: Ensure the change is sustained over time, preventing a return to old practices.
- Phase out the change agent’s role: Gradually reduce the involvement of the change agent, allowing the organization or group to maintain the change independently.
To illustrate how this process might work in the real world, here’s an example of Lippitt’s model in practice:
A nursing home wants to implement a new patient skin care protocol to improve infection control. Cathy, the facility’s director of nursing , is developing a plan following Lippitt’s model. She lays out the steps in her plan below.
- Diagnose the problem: Cathy has noticed that rates of skin infections are higher in her facility than in others. This is a significant concern that warrants action.
- Assess motivation and capacity for change: Cathy assesses her staff’s willingness to adopt new practices and evaluates their training needs, ensuring they have the skills and resources to implement the new protocol.
- Assess the change agent’s motivation and resources: Cathy chooses two of the clinical supervisors from her team to act as change agents, and asks them if they feel equipped for this role. They agree and feel confident they can improve bathing rates.
- Set change objectives: Cathy sets clear, incremental goals for implementing new soap and bathing regimens. She implements regular staff training and creates a system for tracking baths shift-to-shift.
- Choose the role of the change agent: Cathy communicates the clinical supervisor’s roles, and offers staff additional support as changes are made.
- Maintain change: Cathy puts systems in place to monitor adherence to the new protocol, including regular audits and feedback sessions.
- Terminate the helping relationship: Once the new protocol is integrated into daily practices and infection rates improve, the clinical supervisors gradually step back from their change agent roles, allowing the nursing home staff to independently manage and sustain the change.
3. Rogers’ Change Theory
Another popular model is Rogers’ change theory . Nursing innovation happens over time, through communication between members in a social system. Rogers highlights five steps that potential adopters go through. As nursing professionals go through these stages, they can either progress toward change or reject it. The stages are:
- Knowledge: becoming aware of the change, and beginning to understand its function
- Persuasion: people form an opinion about the change, which is often influenced by peers, evidence, and the perceived advantages
- Decision: choosing to adopt or reject the innovation based on the information they have
- Implementation: putting the change into practice
- Confirmation: looking for confirmation that their decision is correct, seeking more evidence that it is the right choice
Rogers’ change theory of nursing also highlights five types of potential adopters when the change process is occurring. Depending on the specific change, and how quickly a person moves through the stages above, every person involved in a change process will fall into one of these categories. These are:
- Innovators: people who drive change themselves; they are risk-takers, willing to try new things
- Early adopters: people who are quick to make a change once they’ve seen others do it, and can endorse the change for others
- Early majority: people who implement changes once they’ve had feedback and modeling from early adopters
- Late majority: a more cautious group that adopts new behaviors once they have been adopted by the majority of the team
- Laggards: the last to adopt an innovation; people who may require penalties in order to change
Trying to get a better understanding of Rogers’ change theory? Nursing examples include:
A hospital is introducing a new medication administration record (MAR). Jennifer hears about this change during a staff meeting ( knowledge phase ). Based on the information she gathers, she is skeptical ( persuasion ).
During training, she tries the new system, and initially finds it hard to work with, but knows she needs to learn it before the old system is phased out ( decision ). She adopts the system in the late majority( implementation ), after she has seen others use it. Once she is comfortable with the new system, she finds that it is easier to work with than the old one, and she is glad the hospital made the change ( confirmation ).
Liam learns about a new evidence-based pain assessment tool in a workshop ( knowledge phase ). He is curious about how it can help him address a patient’s pain more thoroughly ( persuasion ) and wants to try it on his next shift ( decision ). He introduces a patient to the scale ( implementation ) as an early adopter. He later hosts a training for other nurses to help them use the new scale in their practice ( confirmation ).
4. Kotter’s Change Theory
If you’re in a nurse leadership position and you need a framework for leading change, check out Kotter’s change theory . Nursing change, according to change management theorist Dr. John Kotter, happens via an eight-stage process. These stages are:
- Developing urgency: Inspire team members to act.
- Building a guiding team: Select a group of team members to guide change.
- Creating a vision: Communicate the ways that change will be good for everyone.
- Enlisting: Rally team members around the vision.
- Enabling action: Take out roadblocks that slow or stop progress.
- Creating short-term wins: Recognize and reward small amounts of progress.
- Sustain acceleration: Continue to push for change after the first successes.
- Solidify change: Communicate the connection between new behaviors and the success of the organization to solidify change.
Kotter’s change theory doesn’t just describe change as it happens, it also gives managers and nursing leaders a framework for encouraging change. Here’s an example of Kotter’s theory in action:
Mark is a PMHNP who leads a community mental health clinic, and his team is trying to implement a telehealth program to meet the needs of rural patients. He follows Kotter’s steps to promote the adoption of this change:
- Urgency: Mark hosts a meeting to share evidence that patients in their area need more remote care solutions. He has acquired county funding for this initiative, and he sets a deadline for when this new solution must launch.
- Guiding Team: Mark selects two other NPs and their clinic’s IT manager to help him coordinate this change.
- Vision: Mark develops specific goals for this program, outlining how remote psychiatric care will increase access, reduce costs, and decrease acute psychiatric needs.
- Communication: Mark hosts a webinar to explain the vision, attaching a detailed infographic for how this plan will be implemented.
- Enlisting: Staff are trained in using the telehealth system, and are given handouts that they can disseminate to their patients.
- Short-term wins: Mark tracks how many patients enroll in the program, and sends staff congratulatory emails when 20 patients have signed up.
- Sustain: Based on early enrollment, Mark takes feedback and makes it easier for residents to schedule appointments and fill prescriptions from their telehealth app.
- Solidify: Over time, the community learns to lean on telehealth psychiatric support for their mental health needs, and Mark’s clinic integrates remote care training into their onboarding process.
Change Nursing Roles With IntelyCare
Looking to see yourself experience change theory? Nursing offers endless opportunities to grow and alter your skillset. If you’re in the market for new nursing skills and experiences, sign up for personalized job notifications from IntelyCare.
Related Articles
What is a nurse’s role in informed consent, faye abdellah nursing theory explainer and example, patricia benner nursing theory: guide for today’s nurses, networking in nursing: 10 tips to get connected, who is imogene king nursing theory explainer, related jobs.
The university of tulsa Online Blog
Trending topics in the tu online community
Change Theory in Nursing: How It Is Evolving the Profession
The health care industry is constantly evolving. Technical innovations, medical breakthroughs, legal compliance shifts, and new patient care theories can quickly reshape care delivery. For facilities that strive to provide quality care on an optimal level, keeping up with the rapid pace of change requires strict adherence to effectively manage the process of adapting and adjusting. Without such a plan, implementing changes can be less effective.
Effectively managing change is crucial in the nursing field, since nurses are often the first line of patient care. For nurse leaders, the first step in deploying impactful change management within a facility’s nursing team is to have a full understanding of change theory in nursing. Having this understanding can help them interpret the short- and long-term ramifications of each change accurately. This can allow them to make the decisions that can lead to guiding changes that can potentially lead to the highest quality of care delivery possible. For nurses seeking to use their nursing degrees to advance their careers, demonstrating an understanding of change theory may also allow them to stand out.
What Is Change Theory?
Change theory is a viewpoint that aims to manage health care changes in its many forms so that quality patient care remains constant and is not disrupted. These changes come from many directions, including organizational practice, patient care models, care policies, and legal compliance. Using the theory allows health care leaders to govern change management in health care more deliberately, which can lead to cleaner change implementation.
Modern change theory encompasses different principles that can help nurses shape their approach to change management more pragmatically. However, its origins stem from German-American psychologist Kurt Lewin. A pioneer in the field of group dynamics — so much so that he coined the term — Lewin developed change theory as a means to examine how people adapt and adjust to changes within an organization. The principles of change theory can set the framework for nurse leaders to develop strategies to implement change that cause minimal workforce issues.
Breakdown of Lewin’s Change Theory
Lewin’s Change Theory comprises three distinct stages:
- Unfreeze. At the unfreeze stage, an organization decides to make changes that impact employee responsibilities. These changes can disrupt an employee’s routines and methodologies. Some workers may prefer not to have their routines disturbed. To prevent resistance, it is critical to present changes in a way that allows them to mentally prepare themselves for the change.
- Change. At the change stage, most employees have accepted the changes to come. They also display a willingness to learn how to integrate the changes within their daily tasks. This stage is when operational slowdowns may occur, as people may have to get used to the changes. Organizational leaders may keep watch on employee progress at this stage.
- Refreeze. At the refreeze stage, work gets back to normal speed as employees gain familiarity with the changes. When this occurs, organizational leaders develop strategies to enforce and fortify these changes through their various policies and procedures.
Lewin’s Change Theory is vital because it breaks down any change into distinctive sections that can be analyzed and streamlined. For example, the theory compels leaders to think about the level of pushback they may receive from a change; this can help them incorporate ideas that may minimize pushback. It can also help organizations set key performance indicators (KPIs) or benchmarks to chart the progress of each employee impacted. Additionally, it can provide organizations with the vision needed to make changes permanent.
Lewin’s Force Field Analysis: Driving and Restraining Forces
Lewin also developed a sister theory that can help organizations determine whether implementing change makes any sense. This theory, known as the force field analysis, focuses on driving and restraining forces: internal and external influencers surrounding a potential need for change.
Driving forces are the productive factors that can potentially spur development, growth, and progress. These factors ultimately aim to streamline an organization’s progress toward a positive goal. Common driving forces include the following:
- Increased demand
- New federal or state laws
- Managerial pressure
- Public perception
- Field competition
Restraining forces are the factors that can inhibit progress and innovation. These can compel an organization to maintain the status quo and keep the current pace toward goals stable. Common restraining forces include the following:
- Company culture
- Employee unions
- Concerns about the future
- Past unsuccessful change initiatives
According to Lewin’s theory, when these forces are in balance, an organization is in equilibrium and does not need to engage in change. On the other hand, if there is instability between these forces, changes may be inevitable to restore balance.
These different theories can help an organization make more assured decisions on when it may be time to make a change. It can also equip them with the preparedness needed to brace for resistance, provide appropriate guidance, and turn a new idea into a new standard without causing much disruption.
The Uniqueness and Importance of Change Theory in Nursing
The framework of Lewin’s theory applies to a wide range of industries. It has a unique application in nursing because of the field’s purpose. In other organizations, a slowdown in operations due to change adaptation correlates to goods and services. In nursing, it correlates to patient care. This makes it particularly important for nurse leaders to understand change theory.
A lack of understanding of change theory in nursing can leave a nurse leader unprepared for the resistance to change that may come from staff. It can also cause the implementation and permanency of changes to occur more slowly, which can cause a greater disruption to operational processes. This can reduce the efficiency of patient care and make it harder for facilities to achieve their goal of providing care that improves patient outcomes.
The need to engage in change management can come from many different elements. It can come from a new piece of technology that can improve operational efficiency, such as electronic health records (EHRs). It can come from the need to adjust specific procedural elements to comply with new federal or state regulations regarding patient care. It can also be the result of an internal philosophical switch, such as a transition to an evidence-based practice model to improve cost efficiency. These elements can cause different forms of change; addressing and managing these changes in a way that minimizes disruption is essential.
Applying the Stages of Change Theory in Nursing
The application of Lewin’s three stages of change theory is a popular strategy for nurses to use because health care tends to be in constant flux. With each innovation, breakthrough, or new care delivery philosophy, nurse leaders must evaluate the impact of bringing a change into their facility’s environment and ultimately determine if it is needed. This is where the force field analysis can come into play.
A nurse leader can determine whether their facility is in a state of homeostasis, in which patients are consistently receiving optimal care and the facility’s operations and budgets are strong. If it is determined that the facility is out of balance, then change may likely be needed.
The one time that the force field analysis does not potentially factor into this situation is in legal compliance situations. For example, if the federal government were to make a change to its privacy laws, health care facilities would need to adhere to these changes. In these cases, nurse leaders would move directly to applying change theory strategies without needing to analyze whether change is necessary.
Nurse leaders who apply Lewin’s Change Theory can use health care’s penchant for constant change and progress to their advantage.
- At the unfreeze stage , they can prepare staff members for any change by reminding them of the field’s ebb and flow. This can help staff members acknowledge that changes to various processes or the implementation of new technologies come from a place of moving care delivery forward. This step can also involve breaking down how the issues can be fixed or what processes can be improved with the proposed changes.
- At the change stage , nurse leaders can implement various strategies that can allow their staff members to actively engage in the process. For example, leaders can use a transition to an EHR model as an opportunity to help their staff members improve the technical skills associated with using the program. They can also engage them in a way that allows them to take an active role in the implementation. This can involve using group activities, such as coaching and training, to get them comfortable with new processes. This can lower resistance to change and provide an opportunity to showcase the benefits of change.
- At the refreeze stage , nurse leaders must assess the effect that the changes have on the staff members and its ability to deliver optimal patient care. This assessment allows leaders to tweak their strategies to improve integration. Some of these strategies can induce additional training to strengthen weak points and measure KPIs to monitor appropriate progress.
Successfully using change theory to govern care delivery fluctuations can allow nurse leaders to build a strong, trusted rapport with their staff members. This can make it easier for them to function more cohesively, which can improve care efficiency and lead to a more streamlined clinical experience for patients. This rapport can also make them better prepared to roll with the constant changes associated with the health care industry, which can also help change integration occur with minimal disruption to care delivery strategies.
Other Nursing Change Theories
While Lewin’s Change Theory represents the gold standard of change theory in nursing, other theories can help nurses effectively deploy change management in health care while mitigating the potential for jumbling up the patient care process. Most of these theories build off Lewin’s original theory, expanding on its principles to emphasize different areas of change management. Nurse leaders need to also be cognizant of these theories, as they may be able to draw on their philosophies to develop their own pragmatic change management strategy.
Lippitt’s Seven-Step Change Theory
Psychologist Ronald Lippitt augmented Lewin’s original change theory with a few steps. The steps intend to place greater emphasis on the individual promoting the change.
- Step 1: Becoming aware of the need for change after examining all angles of a particular problem
- Step 2: Evaluating resources needed to conduct proper change implementation, such as financial and human capital
- Step 3: Assessing the motivation behind the change
- Step 4: Setting goals and creating action plans to meet goals
- Step 5: Implementing the change, working with staff to ensure a clear understanding of a plan’s parameters
- Step 6: Gathering feedback on change from affected parties
- Step 7: Transitioning from implementation to permanency
Spradley’s Change Theory
Spradley’s Change Theory is also based on Lewin’s original theory but breaks it down into eight steps. This theory emphasizes evaluating the change during the implementation phase to ensure its effectiveness.
- Step 1: Recognize the symptoms that spur the need for change.
- Step 2: Diagnose the issue to build a targeted change strategy.
- Step 3: Analyze change-based solutions.
- Step 4: Select the change solution that works best.
- Step 5: Create a plan to implement the change.
- Step 6: Implement the change.
- Step 7: Assess the change to determine what works.
- Step 8: Stabilize the change before it is made permanent.
Rogers’ Diffusion of Innovation Theory
Everette Rogers’ Diffusion of Innovation theory, a variation of Lewin’s original theory, has five stages. It intends to focus on the reaction of the parties affected by the change, emphasizing the notion that not all individuals involved with the change will adapt to the change simultaneously.
- Stage 1: Inform affected parties about the reason for the change, the process of change implementation, and who will be involved with making these changes.
- Stage 2: Persuade affected parties to accept the change, noting the negative and positive attitudes of those impacted by the change.
- Stage 3: Deploy a pilot program or trial study to determine whether the change should be used.
- Stage 4: Implement change on an established or a permanent basis.
- Stage 5: Confirm change adaptation via feedback from those implementing and impacted by the change.
Bridges’ Theory Into Transition
The Bridges Transition Model is a three-step process that approaches change theory from the affected party’s perspective rather than the change agent’s. Like Rogers’ theory, it gauges the affected party’s reaction, but it emphasizes how the change transforms the individual during and after the change.
- Step 1: Discussing the end goal to signify the change
- Step 2: Gauging the transition between the old ways and new ways of doing things
- Step 3: Acknowledging the new direction via adaptation
Whatever theory a nurse leader uses, they must do so by bringing the Theory of Human Caring into the mix as a supporting player. Developed by registered nurse Jean Wilson, the theory emphasizes the need to ensure that every change is done with the patient’s healing journey at the forefront; this is ultimately established by protecting a caring environment. By incorporating this theory with other change theories, nurse leaders can ensure that their strategies ultimately revolve around caring for the patient. If this suffers, the implemented change ultimately fails.
Become an Impactful Leader of Change
Change theory in nursing carries extra weight compared with change theories in other industries because patient health is involved. Nurse leaders who know how to effectively build change management strategies around these theories can help a health care facility maintain steady quality care while changes occur. In an industry known for its constant change, having this knowledge is key to success in the industry.
The University of Tulsa’s nursing programs can help you develop into a trusted nursing professional who can provide care with the utmost confidence. Our programs are designed to help you advance your nursing career at every phase, whether you’re just starting on your nursing journey or ready to make the bold step into nursing leadership. Learn how we can help you shape your path in this essential field.
Recommended Readings
The Importance of Evidence-Based Practice in Nursing
The Most Important Leadership Skills for Nurses
3 Reasons to Expand Your Nursing Scope of Practice
American Nurses Association, “Current Theories of Change Management”
Indeed, Lewin’s Force Field Analysis (With How to Conduct One)
Indeed, What Is Lewin’s Change Theory? 3-Stage Change Management
Journal of Healthcare Leadership , “Where Do Models for Change Management, Improvement and Implementation Meet? A Systematic Review of the Applications of Change Management Models in Healthcare”
Practical Psychology, Lewin’s Change Theory (Definition + Examples)
Securiti, A Guide to Healthcare Compliance Regulations
SimpleNursing, What Is Change Theory?
StatPearls , “Change Management”
Recent Articles

Is Oklahoma a Compact Nursing State?
University of Tulsa
Jan 13, 2025

Nurse Work Environments: How an MSN Can Broaden Opportunities
Jan 7, 2025

RN to BSN: Requirements for Prospective Students
Learn more about the benefits of receiving your degree from the university of tulsa.
- Online Program Tuition
- AGACNP Certificate Online
- Online MSN Program
- Accelerated Online BSN
- RN to BSN Program
- RN to MSN Program
- MS in Cyber Security
- Meet the Team
- Nursing Student Practicum Requirements
- Disclosures for Professional Nursing Licensure
- On Campus Programs
Want to create or adapt books like this? Learn more about how Pressbooks supports open publishing practices.
9 Common Change Theories and Application to Different Nursing Situations
Sonia A. Udod and Joan Wagner
Leaders take us to places we’ve never been before. But there are no freeways to the future, no paved highways to unknown, unexplored destinations. There’s only wilderness. To step into the unknown, begin with the exploration of the inner territory. We continue to discover that the most critical knowledge for all of us—and for leaders especially—turns out to be self-knowledge . ( Kouzes & Posner, 2007, p. 346 )
Introduction
Change is an essential component of nursing practice. Leading change is a challenge for nurse leaders amid the complexities and challenges of evolving health care environments in providing quality patient care. This chapter is designed to provide nurse leaders with guidance through various theories and frameworks to effectively support the change process in shaping healthy work environments. Additionally, you will learn about resistance to change and how to respond constructively to change. This chapter focuses on providing guidelines for nurse leaders on behaviours and practices for encouraging and facilitating change in the health care setting.
Learning Objectives
- Explain why nurses have the opportunity to be change agents.
- Identify how different theorists explain change.
- Discuss how the nursing process is similar to the change process.
- Discuss the medicine wheel as a change model.
- Describe the nurse leader’s role in implementing change and the call to action.
- Differentiate among change strategies.
- Recognize how to handle resistance to change.
The rapid pace of change in Canada’s health care system provides opportunities for nurse leaders to refine and advance their leadership and management skills for advancing change. Various forces that drive change in health care include rising costs of treatment, new technologies, advances in science, workforce shortages, and an aging population. Change initiatives must always be implemented for good reason within the context of advancing institutional goals and objectives. Balancing change is a key challenge within a patient- and family-centred model to provide safe and reliable patient care ( Stefancyk, Hancock , & Meadows, 2013; Saskatchewan Ministry of Health, 2011 ).
9.1 The Nurse Leader as Change Agent
Nurse leaders must ensure the day-to-day operation of their unit(s) in a rapidly evolving health care system. Nurse leaders are often called upon to be agents of change and are often responsible for the success of a project. Yet the literature suggests that leaders continue to struggle with change despite the frequency with which they are involved in leading change ( Gilley, Gilley, & McMillan, 2009; Quinn, 2004 ). A change agent is an individual who has formal or informal legitimate power and whose purpose is to direct and guide change ( Sullivan, 2012 ). This person identifies a vision and rationale for the change and is a role model for nurses and other health care personnel.
Nurse leaders’ behaviours influence staff actions that contribute to change ( Drucker, 1999; Yukl, 2013 ). The significant number of changes that nurse leaders face require new ways of thinking about leading change and adapting to new ways of working. Moreover, leaders work closely with frontline care providers to identify necessary change in the workplace that would improve work processes and patient care. As such, nurse leaders must have the requisite skills for influencing human behaviour, including supervisory ability, intelligence, the need for achievement, decisiveness, and persistence to guide the process ( Gilley et al., 2009 ). Effective change management requires the leader to be knowledgeable about the process, tools, and techniques required to improve outcomes ( Shirey, 2013 ).
9.2 Theories and Models of Change Theories
Knowledge of the science of change theory is critical to altering organizational systems. Being conversant with various change theories can provide a framework for implementing, managing, and evaluating change within the context of human behaviour. Change theories can be linear or non-linear; however, even linear theories do not unfold in a systematic and organized pattern. In the following section, we identify the role of leader and the typical pattern of events that occur in a change event.
Force Field Model and The Unfreezing-Change-Refreezing Model
Kurt Lewin (1951) is known as a pioneer in the study of group dynamics and organizational development. He theorized a three-stage model of change (unfreezing-change-refreezing model) in order to identify and examine the factors and forces that influence a situation. The theory requires leaders to reject prior knowledge and replace it with new information. It is based on the idea that if one can identify and determine the potency of forces, then it is possible to know the forces that need to be diminished or strengthened to bring about change ( Burnes, 2004 ).
Lewin describes behaviour as “a dynamic balance of forces working in opposing directions” (cited in Shirey, 2013, p.1 ). The force field model is best applied to stable environments and he makes note of two types of forces: driving forces and restraining forces. Driving forces are those that push in a direction that causes the change to occur or that facilitate the change because they push a person in a desired direction. Restraining forces are those that counter the driving force and hinder the change because they push a person away from a desired direction. Finally, change can occur if the driving forces override or weaken the restraining forces.
This important force field model forms the foundation of Lewin’s three-stage theory on change (1951) (see Figure 9.2.1 ). Unfreezing is the first stage, which involves the process of finding a method to assist individuals in letting go of an old pattern of behaviour and facilitating individuals in overcoming resistance and group conformity ( Kritsonis, 2005 ). In this stage, disequilibrium occurs to disrupt the system, making it possible to identify the driving forces for the change and the likely restraining forces against it. A successful change ultimately involves strengthening the driving forces and weakening the restraining forces ( Shirey, 2013 ). This can be achieved by the use of three methods: (1) increase the driving forces that direct the behaviour away from the existing situation or equilibrium; (2) decrease the restraining forces that negatively affect the movement away from the current equilibrium; or (3) combine the first two methods.
The second stage, moving or change , involves the process of a change in thoughts, feelings, and/or behaviours. Lewin (1951 ) describes three actions that can assist in movement: (1) persuading others that the status quo is not beneficial and encouraging others to view a problem with a fresh perspective; (2) working with others to find new, relevant information that can help effect the desired change; and (3) connecting with powerful leaders who also support the change ( Kristonis, 2005 ). This second stage is often the most difficult due to the fact that there is a level of uncertainty and fear associated with change ( Shirey, 2013 ). Therefore, it is important to have a supportive team and clear communication in order to achieve the desired change.
Lastly, stage three, which Lewin called r efreezing , involves establishing the change as a new habit. The third stage is necessary to ensure that the change implemented (in the second stage) will “stick” over time ( Kristonis, 2005 ). Success at this stage will create a new equilibrium state known to be the new norm or higher level of performance expectation ( Shirey, 2013 ).
Although Lewin’s model on change is well known and widely accepted in health care settings, it is often criticized for being too simplistic and linear. Change is often unpredictable and complex, and an effective leader must be aware of many change models.
Figure 9.2.1 The Steps of the Unfreezing-Change-Refreezing Model
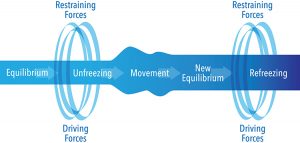
9.3 Planned Change
Lippitt, Watson, and Westley (1958 ) focus more on the role and responsibility of the change agent than on the process of the change itself. Their theory expands Lewin’s model of change into a seven-step process and emphasizes the participation of those affected by the change during the planning steps ( Kritsonis, 2005; Lippitt et al., 1958 ). The seven steps of the planned change model include: (1) diagnosing the problem; (2) assessing the motivation and capacity for change in the system; (3) assessing the resources and motivation of the change agent; (4) establishing change objectives and strategies; (5) determining the role of the change agent; (6) maintaining the change; and (7) gradually terminating the helping relationship as the change becomes part of the organizational culture (see Table 9.3.1 ).
The steps in this model place emphasis on those affected by the change, with a focus on communication skills, rapport building, problem-solving strategies, and establishing mechanisms for feedback ( Kritsonis, 2005; Lehman, 2008 ).
Phases of Change
Ronald Havelock (1973 ) also modified Lewin’s model of change to include six phases of change from planning to monitoring (see Table 9.3.1 ). It is believed that Havelock further developed the unfreezing-change-refreezing model to address two social forces that were gaining momentum in society at the time: “the explosion of scientific knowledge, and the increasing expectation by policy-makers, governments, business and society that scientific knowledge should be useful to society” ( Estabrooks, Thompson, Lovely, & Hofmeyer, 2006, pp. 29–30 ). Havelock argued that adapting Lewin’s change model to include knowledge building, which focused on a systematic integration of theories rather than disjointed approaches, would respond more effectively to real-life situations in managing change ( Estabrooks et al., 2006 ).
The six phases of Havelock’s model are as follows:
- Building a relationship . Havelock regarded the first step as a stage of “pre-contemplation” where a need for change in the system is determined.
- Diagnosing the problem . During this contemplation phase, the change agent must decide whether or not change is needed or desired. On occasion, the change process can end because the change agent decides that change is either not needed or not worth the effort.
- Acquire resources for change . At this step, the need for change is understood and the process of developing solutions begins as the change agent gathers as much information as possible relevant to the situation that requires change.
- Selecting a pathway for the solution . A pathway of change is selected from available options and then implemented.
- Establish and accept change . Individuals and organizations are often resistant to change, so careful attention must be given to making sure that the change becomes part of new routine behaviour. Effective communication strategies, staff response strategies, education, and support systems must be included during implementation.
- Maintenance and separation . The change agent should monitor the affected system to ensure the change is successfully stabilized and maintained. Once the change has become the new normal, the change agent can separate from the change event. ( Tyson, 2010 )
Innovation Diffusion Theory
Rogers’ five-step theory explains how an individual proceeds from having knowledge of an innovation to confirming the decision to adopt or reject the idea (see Figure 9.3.1 ) ( Kritsonis, 2005; Wonglimpiyarat & Yuberk, 2005 ). A distinguishing feature of Rogers’ theory is that even if a change agent is unsuccessful in achieving the desired change, that change could be resurrected at a later, more opportune time or in a more appropriate form ( Kritsonis, 2005 ). Roger also emphasizes the importance of including key people (i.e., policy-makers) interested in making the innovation happen, capitalizing on group strengths, and managing factors that impede the process. The five stages to Rogers’ theory are as follows:
- Knowledge . The individual is first exposed to an innovation but lacks information about the innovation.
- Persuasion . The individual is interested in the innovation and actively seeks related information and details.
- Decision . The individual considers change and weighs the advantages and disadvantages of implementing the innovation.
- Implementation . The individual implements the innovation and adjusts the innovation to the situation. During this stage the individual also determines the usefulness of the innovation and may search for further information about it.
- Confirmation . The individual finalizes the decision to continue using the innovation. ( Rogers, 1995 )
Essential Learning Activity 9.3.1
Watch the video “ Lewin’s 3-Stage Model of Change: Unfreezing, Changing & Refreezing ” (8:06) by Education-Portal.com for more about Lewin’s change model.
Watch the video “ Rogers Diffusion of Innovation ” (3:15) by Kendal Pho, Yuri Dorovskikh, and Natalia Lara (Digital Pixels) for more about Rogers’ theory of innovation.
Figure 9.3.1 The Five Steps of the Innovation Decision Process

Rogers’ innovation diffusion theory explains how, why, and at what rate new ideas are taken up by individuals. Rogers defines five-categories of innovation adopters. Innovators are willing to take risks; they are enthusiastic and thrive on change. They play a key role in the diffusion of innovation by introducing new ideas from the external system ( Rogers, 1995 ). Early adopters are described as being more discreet in adoption choices than innovators. They are cautious in their adoption of change. The early majority are those people who take a significantly longer time to adopt an innovation as compared to the innovators and early adopters. The late majority comprise individuals who have a high degree of skepticism when it comes to adopting a change. Finally, the laggards are those who are last to adopt a change or innovation. They typically have an aversion to change and tend to be focused on traditions and avoid trends ( Rogers, 1995 ).
9.4 Non-linear Change Models
Most organizations have viewed change as sequential and linear occurring in a step-by-step fashion. However, nursing has begun to explore non-linear models as a way of guiding more unpredictable change, as these models do not follow an orderly and predictable pattern.
Chaos Theory
Chaos theory, considered to be a subset of complexity science, emerged from the early work of Edward Lorenz in the 1960s to improve weather forecasting techniques. Non-human-induced responses in the environment indicate there is some predictability in random patterns ( Thietart & Forgues, 1995; Wagner & Huber, 2003 ). Lorenz found that even small changes of randomness in a system that constantly changes can dramatically affect the long-term behaviour of that system and make it difficult to predict future outcomes. Interestingly, this non-linear model refers to a controlled randomness, which may be associated with recognizable and somewhat predictable patterns.
Chaos theory may be another way to structure change processes in a highly complex and evolving health care environment. Despite the best of intentions to improve organizational function and improve quality and safety of patient care, contextual factors may not be fully explored or considered in the change process. For example, instituting a care delivery model on a unit may not work well if staff have not been appropriated the necessary resources to provide care. Knowing how non-linear theories work can advance organizational functioning in health care organizations and systems in the twenty-first century.
Essential Learning Activity 9.4.1
Watch Claire Burge’s TEDx Talk titled “ The Future of Work is Chaos ” (13:43) for a more in-depth understanding of chaos theory.
Essential Learning Activity 9.4.2
Cindy is an RN with three years’ experience working on a busy surgical unit in a large urban hospital. Cindy enjoys her job and is keen to pursue an intensive care course after which she plans to work in the intensive care unit of the same hospital. She has received a one-year grant to establish a cardiac program for patients and caregivers. This project will be evaluated at the end of one year. Cindy, as the change agent, is tasked with implementing the change. Stephanie, the nurse manager, is highly supportive, but some of the nurses don’t have time and are not willing to help make the program a reality.
How should Cindy proceed with the change process? Could Lewin’s change theory be used to guide the change? If so, how would you envision the change occurring?
How can she persuade other nurses to buy into the change? What effective leadership and followership strategies could she implement in the change process?
9.5 The Nursing Process as the Change Process
The change process can be related to the nursing process and is described by Sullivan ( 2012 ) in four steps. Assessment , the first step, entails identifying the problem. It involves collecting and analyzing data. Pinpointing the problem enables individuals affected by a proposed change to have a clear and accurate understanding of the problem.
Once the problem is identified, the change agent collects external and internal data as needed (e.g., patient satisfaction questionnaires, staff surveys). A critical analysis of the data supports the need for change, at which point the change agent determines resistance, identifies potential solutions, and begins to develop consensus regarding change. Assessing the political climate by determining who will benefit from the change, accessing resources, and having credibility with and respect of the staff will enhance the leader’s ability to increase the driving forces and reduce the restraining forces ( Lewin, 1951 ). Sullivan (2012 ) recommends converting data into tables or graphs, thus making the results easier for administration and frontline providers to understand, and perhaps accept, the change.
Planning requires the participation of staff that will be affected by the change. Relationships among staff may be altered if structures, rules, and practices are modified. This in turn alters workforce requirements, which may then lead to hiring new people with different skills, knowledge, attitudes, and motivations ( Sullivan, 2012 ). It is anticipated that less resistance will be encountered if staff are involved at the planning stage, since attitudes, ways of thinking, and behaviours need to shift to accommodate a new way of working.
Weiss and Tappen (2015 ) recommend three tactics that can be used to unfreeze members or staff. First, sharing information is a way to help staff understand the rationale for a proposed change. Second, disconfirming currently held beliefs is a way to demonstrate that a current goal of the target system is inadequate, incorrect, or inefficient and therefore needs to be modified. Third, providing psychological safety is a tactic that minimizes risk by affording sufficient security to staff. This tactic is highly valuable as it generates a feeling of security and facilitates members’ ability to trust and accept the change. These three tactics decrease anxiety about the change. Establishing target dates and time frames to determine progress and providing opportunities for members to offer feedback will support the change.
In the implementation stage, plans are put into action. The change agent sets the tone for a positive and supportive climate, and methods are used to continue persuading members toward the change (providing information, training, assisting with personnel changes). Strategies are used to change the group dynamics to encourage members to act based on group decisions.
During evaluation , indicators are monitored to determine whether goals have been met, and what, if any, undesirable outcomes occurred and how to respond to unintended consequences. Once the desired outcome is reached, the change agent terminates the role by delegating responsibilities to members. Policies and procedures may be necessary to stabilize the change as part of everyday practice. The leader, as energizer and supporter, continues to reinforce behaviours through ongoing feedback.
9.6 The Medicine Wheel as a Change Model
The medicine wheel, drawn as a circle with four quadrants, represents a holistic set of beliefs encompassing the mind , body , emotions , and spirit , which is foundational to the human being. These beliefs have been embraced by Indigenous cultures across the world for thousands of years ( McCabe, 2008 ). Carl Jung and others emphasized this dialogue between the four aspects of the human being as a way to understand self and maintain health ( McCabe, 2008 ). Psychologists recognize the medicine wheel as “the Jungian mandala—a symbol of wholeness” ( Dapice, 2006, p. 251 ).
Figure 9.6.1 Medicine Wheel
The medicine wheel is found in the teachings of individual Elders in over 500 Indigenous nations across Canada. Teachings are similar between the nations; however there are slight differences regarding the location of the four dimensions on the wheel ( Clarke & Holtslander, 2010 ). The medicine wheel is manifested within the community as a “process (healing), a ceremony (sweats, sharing circles) and teachings (a code for living)” ( McCabe, 2008, p. 34 ). The Indigenous people consider the community participation in ceremonies to be an important part of the healing process ( McCabe, 2008 ). The medicine wheel assists community members to connect with each other, while also supporting balance and harmony across the four dimensions of mind, body, emotions, and spirit for the individual and the extended community ( Clarke & Holtslander, 2010 ).
Recent literature focuses on the use of the medicine wheel to recover from illness and regain health. The medicine wheel guides healthy change and can be individualized to the specific needs of the client or community , taking into account the context of culture, socioeconomic status, family situation, disease process, and other significant factors, culminating in balance, healing, and growth in all four aspects. Research literature documents the use of the medicine wheel in diabetes education ( Kattelmann , Conti, & Ren , 2010 ), end-of-life care for Aboriginal people ( Clarke & Holtslander, 2010 ), substance abuse prevention programs ( Walsh-Buhl, 2017 ), adolescent group counselling ( Garner , Bruce, & Stellern , 2011 ), and development of a retention program for diverse nursing students ( Charbonneau-Dahlen, 2015 ). The medicine wheel provides a guide to holistic change for both the individual and the collective community.
Essential Learning Activity 9.6.1
Watch the video “ Medicine Wheel: Beyond the Tradition ” (9:20), for an explanation and overview of the Lakota (Sioux) medicine wheel, according to Don Warne, then answer the following questions:
- What does the medicine wheel represent?
- How does the use of the medicine wheel extend from traditional to modern times?
- Which gifts come from each of the four directions?
9.7 The Nurse Leader’s Role in Managing Organizational Change
The nurse leader’s role as change agent is complex and varied in nature, and it represents significant leadership challenges. Innovative organizational change can be effectively managed with proven leadership strategies and tools ( MacPhee, 2007 ). The change agent has two main responsibilities: to change oneself and to build capacity in others. Stefancyk et al. (2013 ) introduced the idea of a change coach , which builds upon the traditional role of a nurse leader. A change coach or leader uses coaching behaviours that include guidance, facilitation, and inspiration ( Stefancyk et al., 2013 ). The leader uses guidance to set behavioural expectations for staff performance and provides feedback on performance in the change project. As a facilitator, the change coach encourages staff to share in decision making, thereby creating and nurturing a culture that supports input from others, facilitates creative thinking, and enhances the process of finding the best solutions to address challenges. The leader takes on an inspirational role, expressing confidence and recognizing staff as providing meaningful contributions to the change process.
Building partnerships with staff that include two-way communication, both internally and externally, is critical to building trust and teamwork ( Gilley et al., 2009; Yukl, 2013 ). Communication strategies can include informing those affected by the change how the change will affect their job, and providing information in a timely manner to help them make effective decisions. Nurse scholars ( MacPhee, 2007; Morjikian, Kimball , & Joynt, 2007; Stefanyk et al., 2013 ) suggest that developing trust is a component of communicating effectively, and that this can be accomplished through demonstrating approachability, building rapport, listening, and restating the opinions of others (even when the leader disagrees with the opinion). Listening to staff also means being aware of change fatigue , a condition experienced by individuals subjected to unrelenting and overwhelming change in their work environments ( Bowers, 2011 ). Leadership and management skills and behaviours can positively influence the execution of change initiatives ( Gilley et al., 2009 ).
A call to action means the leader knows when strategies for change need to be altered to foster effective followership. Navigating complex organizational structures through formal and informal power networks is foundational to setting the stage for a successful change. Organizational agility requires the leader to know and understand how the organization works and to be familiar with key policies, practices, and procedures.
9.8 Change Strategies
According to the classic model developed by Bennis , Benne, and Chinn (1960 ), three strategies can be used to facilitate change. The characteristics of the change agent and the amount of resistance encountered will determine which of the following strategies should be used.
- Power-coercive strategies are based on the application of power through legitimate authority ( Sullivan, 2012 ). Little effort is used by the nurse leader to enforce change, and staff has no ability to alter the course of the change process. Power-coercive strategies can be used when change is critical, time is limited, there are high levels of resistance, and there may be little or no chance of reaching organizational consensus ( Sullivan, 2012 ).
- Empirical-rational strategies assume that providing knowledge is the most powerful requirement for change ( Sullivan, 2012 ). This strategy assumes that people are rational and will act in their own self-interest when they understand that change will benefit them. It can work well if the change is perceived as reasonable or beneficial for individuals.
- Normative-reeducative strategies assume that individuals act in accordance with social norms and values that influence their acceptance of change ( Sullivan, 2012 ). The nurse leader focuses on individual’s behavioural motivators such as roles, attitudes, feelings, and their interpersonal relationships as an effective way to implement change in the health care environment.
9. 9 Response and Resistance to Change
Several factors can influence resistance to change. It is not uncommon for staff to state that they were not involved in the decision making regarding changes in their practice and, as a result, be highly resistant to change. While not everyone will embrace change, individuals respond on a continuum that ranges from a lack of enthusiasm to overt sabotage ( Gaudine & Lamb, 2015 ). Resistance may involve a personal loss, feelings of inadequacy, lack of competence, and lack of confidence to perform ( Austin & Claassen, 2008 ). Leaders who can help members psychologically own the change are more likely to see the change initiative sustained and embedded in practice.
We offer the following strategies to counter resistance:
- Understand that resistance is a natural part of the process but must be constructively addressed for change to progress.
- Learn why an individual is resisting the change. Perhaps the resistance may be related to the lack of understanding in how the change process unfolds, which calls for supporting their ability to adjust to the change.
- Link some of the old ways of working with the new change as a way to bridge the old with the new and bring some familiarity to new practices ( Austin & Claassen, 2008 ).
- Identify people who are willing to try new practices, which can reduce the possible resistance from others when change is introduced ( Bowers, 2011 ).
- Assist staff in identifying with and valuing how the change will affect their practice (i.e., help them to assume ownership for the change) in order to ensure that the change is embraced and sustained.
- Communicate a clear vision of the benefits to be gained from the change ( Yukl, 2013 ). Structured and transparent communication aids the participation and involvement of staff.
One of the most difficult activities for the nurse leader is leading change in an organization. The nurse leader needs to have excellent leadership skills, be conversant with change theories, and be able to partner and work effectively with staff in achieving the vision. Being a change coach involves navigating change, generating and mobilizing resources toward innovation, and improving outcomes.
After completing this chapter, you should now be able to:
- How do you normally respond to change in your personal life? How did you respond to your first clinical situation?
- Identify the leadership skills that a nurse leader must apply when implementing change.
- Identify a change occurring in your workplace. Using one of the change theories presented in this chapter, analyze how well the change process is working.
- What are some of the contributing factors to the failure of change projects?
- Reflect on how you as a follower can be a positive asset to a change process.
Austin, M. J., & Claassen, J. (2008). Impact of organizational change on organizational culture. J ournal of Evid ence- Inf ormed Soc ial Work, 5 (1–2), 321–359. doi:10.1300/J394v05n01_12
Bennis, W., Benne, K., & Chinn, R. (1960). The planning of change (2nd ed.). New York: Holt, Rinehart, & Winston.
Bowers, B. (2011). Managing change by empowering staff. Nursing Times, 107 (32–33), 19–21.
Burnes, B. (2004). Kurt Lewin and complexity theories: Back to the future? Journal of Change Management, 4, 309–325.
Charbonneau-Dahlen, B. K. (2015). Hope: The dream catcher-medicine wheel retention model for diverse nursing students. J ournal of Theory Constr uction and Test ing , 19 (2), 47–54.
Clarke, V., & Holtslander, L. F. (2010). Finding a balanced approach: Incorporating medicine wheel teachings in the care of Aboriginal people at the end of life . J ournal of Palliat ive Care, 26 (1), 34–36.
Dapice, A. N. (2006). The medicine wheel. J ournal of Transcult ural Nurs ing , 17 (3), 251–260.
Drucker, P. (1999). Management challenges for the 21 st century . New York: Harper Collins.
Estabrooks, C. A., Thompson, D. S., Lovely J. J. E., & Hofmeyer, A. (2006). A guide to knowledge translation theory. J ournal of Contin uing Educ ation in the Health Prof essions , 26 (1), 25–36. doi:10.1002/chp.48
Garner, H., Bruce, M. A., & Stellern, J. (2011). The goal wheel: adapting Navajo philosophy and the medicine wheel to work with adolescents. Journal for Specialists in Group Work , 36 (1), 62–77. doi:10.1080/01933922.2010.537735
Gaudine, A., & Lamb, M. (2015). Nursing leadership and managing working in Canadian health care organizations. Toronto: Pearson.
Gilley, A., Gilley, J. W., & McMillan, H. S. (2009). Organizational change: Motivation, communication, and leadership effectiveness. Perf ormance Improvement Q uarterly , 21 (4), 75–94. doi:10.1002/piq.20039
Havelock, R. (1973). The change agent ’ s guide to innovation in education . Englewood Cliffs, NJ: Educational Technology.
Kattelmann, K. K., Conti, K., & Ren, C. (2010). The Medicine Wheel nutrition intervention: A diabetes education study with the Cheyenne River Sioux Tribe. J ournal of the Am erican Diet etic Assoc iation , 109 (9), 44–51. doi:10.1016/j.jada.2010.03.003
Kouzes, J. M., and Posner, B. (2007). The leadership challenge (4th ed.). San Francisco: Jossey-Bass.
Kritsonis, A. (2005). Comparison of change theories. International Journal of Scholarly Academic Intellectual Diversity, 8 (1), 1–7. Retrieved from http://commonweb.unifr.ch /artsdean/pub/gestens/f/as/files/4655/31876_103146.pdf
Lehman, K. L. (2008). Change management: Magic or mayhem? Journal for Nurses in Staff Development, 24 (4), 176–184.
Lewin, K. (1951). Field theory in social sciences . New York: Harper & Row.
Lippitt, R., Watson, J., & Westley, B. (1958). The dynamics of planned change. New York: Harcourt Brace.
MacPhee, M. (2007). Strategies and tools for managing change. The Journal of Nursing Administration, 37 (9), 405–413.
McCabe, G. (2008). Mind, body, emotions and spirit: Reaching to the ancestors for healing. Couns elling Psychol ogy Q uarterly , 21 (2), 143–152. doi:10.1080/09515070802066847
Morjikian, R. L., Kimball, B., & Joynt, J. (2007) Leading change: The nurse executive’s role in implementing new care delivery models. The Journal of Nursing Administration , 37 (9), 399–404. doi:10.1097/01.NNA.0000285141.19000.bc
Quinn, R. E. (2004). Building the bridge as you walk on it . San Francisco: Jossey-Bass.
Rogers, E. (1995). Diffusion of innovations (4th ed.). New York: Free Press.
Saskatchewan Ministry of Health. (2011) Patient- and family-centred care: Putting patients and families first . Retrieved from https://www.saskatchewan.ca/government/health-care-administration-and-provider-resources/saskatchewan-health-initiatives/patient-and-family-centred-care
Shirey, M. (2013). Lewin’s theory of planned change as a strategic resource. The Journal of Nursing Administration, 43 (92), 69–72. doi:10.1097/NNA.0b013e31827f20a9
Stefancyk, A., Hancock, B., & Meadows, M. T. (2013). The nurse manager: Change agent, change coach? Nursing Administration Quarterly, 37 (1), 13–17. doi:10.1097/NAQ.0b013e31827514f4
Sullivan, E. J. (2012). Effective leadership and management in nursing (8th ed.). Upper Saddle River, NJ: Pearson.
Thietart, R. A., & Forgues, B. (1995). Chaos theory and organization. Organization Science, 6 (1), 19–31.
Tyson, B. (2010). Havelock’s theory of change . Retrieved from http://www.brighthubpm.com/change-management/86803-havelocks-theory-of-change/
Wagner, C. M., & Huber, D. L. (2003). Catastrophe and nursing turnover: Nonlinear models. The Journal of Nursing Administration, 33 (9), 486–492.
Walsh-Buhl, M. L. (2017). Please don’t just hang a feather on a program or put a medicine wheel on your logo and think ‘oh well, this will work.’ Fam ily and Community Health, 40 (1), 81–87. doi:10.10 97/FCH.0000000000000125
Weiss, S. A., & Tappen, R. M. (2015). Essentials of nursing leadership and management (6th ed.). Philadelphia: F.A. Davis.
Wonglimpiyarat, J., & Yuberk, N. (2005). In support of innovation management and Roger’s Innovation Diffusion Theory. Gov ernment Inf ormation Q uarterly , 22 (3), 411–422. doi:10.1016/j.giq.2005.05.005
Yukl, G. (2013). Leading in organizations (8th ed.). Upper Saddle River, NJ: Pearson.
Leadership and Influencing Change in Nursing Copyright © 2018 by Joan Wagner is licensed under a Creative Commons Attribution 4.0 International License , except where otherwise noted.
Share This Book

Understanding the 3 Phases of Lewin’s Change Theory in Nursing: A Framework for Successful Transformation
Lewin’s Change Theory stands out as a fundamental framework that has significantly influenced the field of nursing. Developed by psychologist Kurt Lewin in the 1940s, this theory has become a cornerstone for nurses seeking to foster positive change within their organizations.
This article delves into the core principles of Lewin’s Change Theory, its application in nursing practice, and its impact on promoting successful transformation in healthcare settings.
Understanding Lewin’s Change Theory:
What You'll Learn
Kurt Lewin’s Change Theory is based on the belief that change occurs in three distinct stages: unfreezing, moving, and refreezing . Each phase is critical in the successful implementation of organizational change .

The first stage involves preparing the organization or individual for change. During this phase, nurses and healthcare leaders must recognize the need for change and create a sense of urgency. This requires identifying existing practices that may be hindering progress and fostering open communication to gain support from all stakeholders.
Unfreezing is akin to breaking free from the status quo and acknowledging that change is necessary for growth and improvement.
In the context of nursing, unfreezing might entail identifying outdated protocols or processes that no longer align with evidence-based practices. For example, if a hospital has been using paper-based patient records, transitioning to an electronic health record (EHR) system would require unfreezing the mindset of staff members who may be comfortable with the old paper-based system.
Effective communication with the nursing staff and demonstrating the benefits of the EHR system are essential to facilitate the unfreezing process.
Once the organization or individual is unfrozen, the next phase is the transition itself. In this stage, nurses must effectively implement the changes, adopt new practices, and adapt to the transformed environment. Clear and consistent communication plays a pivotal role in keeping everyone informed and engaged throughout the process .
Nurses must also be prepared to address any resistance to change that might arise among staff members, patients, or other stakeholders. This stage often demands strong leadership and the ability to navigate challenges with resilience and adaptability.
In nursing practice, the moving stage could involve the introduction of a new care delivery model, such as the implementation of interprofessional care teams to improve patient outcomes.
During this phase, nurses must collaborate with other healthcare professionals, like physicians, pharmacists, and social workers, to create cohesive care plans for patients. They must also be prepared to handle resistance from some team members who might be hesitant to change their traditional roles.
Read More on How to write a Nursing Change Project
The final stage of Lewin’s Change Theory involves stabilizing the change and solidifying it as the new norm. Refreezing aims to reinforce the positive outcomes achieved during the transition and integrate the changes into the organization’s culture. This may include updating policies and procedures, providing ongoing training and support, and celebrating the successes resulting from the implemented changes.
The goal is to ensure that the new practices become firmly rooted in the organization and are sustained over time.
In the nursing context, refreezing may involve establishing new standard operating procedures (SOPs) for the implemented change and providing continuous education and training to reinforce the new practices. For instance, if the nursing unit has implemented a patient-centered care approach, nurses might undergo periodic workshops and seminars to further enhance their patient communication and engagement skills.
Application of Lewin’s Change Theory in Nursing Practice:
Lewin’s Change Theory has substantial implications for nursing practice, particularly in the context of healthcare settings where change is constant. Nurses can apply this theory to numerous scenarios, such as implementing new evidence-based practices, introducing technological advancements, or restructuring healthcare processes to improve patient outcomes.
- Implementing Evidence-Based Practices:
Incorporating evidence-based practices is vital to enhancing the quality of patient care . Nurses can use Lewin’s Change Theory to educate their colleagues about the benefits of evidence-based approaches, address any resistance to change, and promote a culture that values continuous improvement in nursing care .
Evidence-based practice involves integrating the best available evidence from research with clinical expertise and patient preferences. To implement evidence-based practices successfully, nurses must engage in continuous learning and self-improvement. They can use Lewin’s Change Theory to create an environment that fosters learning and experimentation, empowering nurses to embrace new research findings and adopt evidence-based protocols.
- Embracing Technological Advancements:
As technology continues to revolutionize healthcare, nurses must adapt to new tools and systems. Lewin’s Change Theory can guide the implementation of technology, ensuring a smooth transition and minimizing disruptions to patient care during the learning phase.
For instance, when introducing a new medication administration system, nurses can use Lewin’s Change Theory to assess the readiness of the nursing staff for the change. By identifying potential barriers and resistance, nurses can develop strategies to mitigate challenges and ensure a successful transition to the new system.
Additionally, ongoing support and training are essential during the moving stage to help nurses feel confident in using the technology effectively.
- Restructuring Healthcare Processes:
Streamlining healthcare processes can lead to improved efficiency and patient satisfaction. By using Lewin’s Change Theory, nurses can facilitate the reorganization of workflows and encourage staff members to embrace more effective practices.
For example, in a hospital setting, nurses might work collaboratively with administrators and other healthcare professionals to optimize patient flow and reduce wait times . This could involve redesigning triage processes, implementing a centralized patient admission system, or creating multidisciplinary teams to address specific patient needs.
By applying Lewin’s Change Theory, nurses can guide the entire organization through the change process, ensuring that the revised processes become ingrained in the culture.
Impact on Promoting Successful Transformation:
Lewin’s Change Theory offers a structured and comprehensive approach to managing change in nursing practice. Its application can lead to various benefits, including:
- Increased Staff Engagement:
By involving all stakeholders in the change process, nurses can create a collaborative environment where staff members feel valued and are more likely to embrace change willingly. Engaged nurses are more likely to participate actively in the change effort, leading to smoother transitions and greater acceptance of new practices.
Engagement can be fostered through open communication channels, such as town hall meetings, focus groups, and regular feedback sessions. Nurses can use these platforms to listen to their colleagues’ concerns and suggestions, making them feel like an integral part of the decision-making process.
- Enhanced Patient Outcomes:
Efficiently implementing change can lead to improved patient care and outcomes, resulting in higher patient satisfaction rates and a positive impact on the organization’s reputation. For example, if nurses successfully implement evidence-based care protocols for managing chronic conditions, patients may experience better health outcomes, reduced hospital readmissions, and an improved overall healthcare experience.
By adhering to Lewin’s Change Theory, nurses can ensure that the changes implemented are well-planned, effectively communicated, and supported by the entire care team. This comprehensive approach contributes to better patient care and improved health outcomes.
- Improved Organizational Performance
Nursing teams that successfully navigate change using Lewin’s theory often experience improved productivity, reduced errors, and increased overall organizational performance. A well-managed change process can lead to streamlined workflows, reduced waste, and a more efficient use of resources.
Moreover, nurses who are skilled in managing change are better equipped to address challenges and seize opportunities for continuous improvement. By embedding a culture of change, organizations can become more adaptable and resilient in the face of future healthcare challenges.
Conclusion:
Lewin’s Change Theory continues to be a valuable tool for nursing professionals as they navigate the ever-evolving landscape of healthcare. By understanding and applying the three stages of unfreezing, moving, and refreezing, nurses can lead successful transformation initiatives and positively impact patient care and organizational outcomes. As the healthcare industry continues to evolve, Lewin’s Change Theory remains an essential guide for nurses seeking to embrace change and drive continuous improvement in their practice and the healthcare organizations they serve.
Working On an Assignment With Similar Concepts Or Instructions?
A Page will cost you $12, however, this varies with your deadline.
We have a team of expert nursing writers ready to help with your nursing assignments. They will save you time, and improve your grades.
Whatever your goals are, expect plagiarism-free works, on-time delivery, and 24/7 support from us.
Here is your 15% off to get started. Simply:
- Place your order ( Place Order )
- Click on Enter Promo Code after adding your instructions
- Insert your code – Get20
All the Best,
Post navigation
Previous post.
Change Theory in Nursing: Guide

Ethan is an experienced editor specializing in nursing and academic writing, with over eight years' expertise. He excels in refining complex medical content, research papers, and academic essays.
What Is a Change Theory in Nursing
Change theory in nursing refers to concepts and principles that help nurses understand, plan, and implement change in healthcare settings. To provide optimal care, nursing professionals must adapt to new practices, technologies, and patient care standards in an ever-evolving healthcare landscape.
The importance of the change theory nursing concept cannot be overstated, as it equips nurses with the knowledge and skills to manage change effectively. It includes identifying areas needing improvement, setting achievable goals, and involving team members in the change process. By embracing change theory, nurses can ensure a smoother transition and minimize resistance when implementing new practices, ultimately leading to better patient outcomes and a more efficient healthcare system.
This article aims to provide an overview of change theory in nursing, emphasizing its significance and application in nursing. With a solid understanding of change theory, nurses can become agents of change and contribute to the ongoing evolution of healthcare.
Theoretical Frameworks in Nursing: Building a Strong Foundation for Practice
Theoretical frameworks in nursing are essential as they provide a foundation for nursing practice, research, and education. These change management frameworks consist of concepts, definitions, and propositions that explain and predict various aspects of nursing, enabling nurses to understand the underlying principles of their profession.
The significance of theoretical frameworks in nursing practice is manifold. Firstly, they offer a structured approach to problem-solving, allowing nurses to identify issues, develop evidence-based solutions, and evaluate outcomes. Secondly, these frameworks provide a common language for nursing professionals to communicate their ideas, ensuring consistency and clarity.
Moreover, theoretical frameworks in nursing help bridge the gap between theory and practice by guiding the integration of evidence-based knowledge into daily nursing activities. This results in improved patient care, as nurses are better equipped to understand the complex factors affecting their patients' health and well-being.
Understanding Change: A Key Component in Nursing Evolution
Change in nursing refers to modifying or transforming various aspects of nursing practice, education, research, or administration. It can involve adopting new technologies, updating care protocols, or revising organizational structures to improve patient outcomes and enhance healthcare delivery.
There are several reasons for the change in nursing, including advancements in medical knowledge, technological innovations, evolving patient demographics, and changes in healthcare regulations. Adapting to these changes ensures that nursing practices remain relevant, evidence-based, and responsive to the dynamic nature of the healthcare environment.
Changes in nursing can be categorized into three main types: incremental, transitional, and transformational. Incremental changes are small adjustments that improve existing practices without significantly altering the overall system. Transitional changes involve a more significant shift in processes or structures, often requiring new skill sets and adjustments to established routines. Transformational changes are large-scale, radical modifications that profoundly impact the nursing profession and require a complete overhaul of existing paradigms.
Change Management in Nursing: Guiding Successful Transitions
Nursing change management refers to the systematic approach nursing professionals use to plan, implement, and evaluate change processes within their practice, department, or organization. It is a critical aspect of nursing leadership that ensures changes are executed efficiently and effectively, with minimal disruption to patient care.
The importance of change management theory in nursing lies in its ability to facilitate smooth transitions and minimize resistance to change, which can lead to better patient outcomes, improved teamwork, and enhanced job satisfaction among nursing staff. Effective change management fosters a culture of adaptability, resilience, and continuous improvement within nursing.
The steps involved in change management in nursing typically include the following:
- Identifying the need for change and establishing clear objectives.
- Developing a comprehensive change plan, including timelines and resources.
- Communicating the proposed change to all relevant stakeholders.
- Providing education and training to support the change process.
- Implementing the change and monitoring its progress.
- Evaluating the change outcomes and making necessary adjustments.
- Consolidating the change and reinforcing its value.
Resistance to change in nursing can stem from various factors, such as fear of the unknown, perceived loss of control, or concerns about increased workload. Addressing these concerns through open communication, involving staff in the change process, and providing adequate support can help mitigate resistance and ensure successful implementation.
Change Theories in Nursing: Guiding Principles for Adaptation
Change theories in nursing provide a framework for understanding, planning, and implementing change in healthcare settings. These theories offer valuable insights into the change process, enabling nursing professionals to manage change effectively and efficiently. Lewin's Change Theory and Rogers' Change Theory are prominent change theories in nursing.
Lewin's Change Theory: Navigating the Change Process
Lewin's Change Theory, developed by psychologist Kurt Lewin, is a widely used model for understanding and managing change. This theory describes the change process as a series of three stages: Unfreezing, Change (or Moving), and Refreezing.
- Unfreezing: This stage involves creating awareness of the need for change, addressing resistance, and preparing individuals for the upcoming transition.
- Change (Moving): In this stage, the actual change is implemented, requiring individuals to learn new behaviors, adopt new practices, and adapt to the new situation.
- Refreezing: The final stage focuses on stabilizing the change and reinforcing new behaviors to ensure they become a permanent part of the system.
Lewin's Change Theory can be applied in nursing to guide the implementation of new practices or technologies, such as transitioning from paper-based documentation to electronic health records. Following the three stages, nursing professionals can minimize resistance, support the learning process, and establish a solid foundation for lasting change.
Rogers' Change Theory: Embracing Innovation
Rogers' Change Theory, also known as the Diffusion of Innovations Theory, was developed by Everett Rogers and focused on how innovations spread within a social system. This theory emphasizes the role of communication, social networks, and individual characteristics in adopting new ideas for change in nursing practice.
Key concepts of Rogers' Change Theory include:
- Innovation: A new idea, practice, or technology adopter perceives as a novel.
- Communication channels: The means through which information about the innovation is exchanged among individuals.
- Time: The duration required for individuals to adopt or reject the innovation.
- Social system: The interconnected network of individuals who influence one another's adoption decisions.
Rogers' Change Theory can be applied in nursing to understand how new practices or technologies are adopted within a healthcare setting. For example, when introducing a new wound care technique, nursing leaders can use this theory to identify early adopters, facilitate communication, and address barriers to adoption.
The Transtheoretical Model: A Journey Through Change
The Transtheoretical Model (TTM), developed by Prochaska and DiClemente, is a psychological model that describes the process of intentional behavior change. It emphasizes that change is a dynamic, multi-stage process rather than a one-time event. TTM is useful in understanding individuals' readiness for change and tailoring interventions accordingly.
The TTM comprises five stages of change:
- Precontemplation: Individuals are not yet aware of the need for change or are resistant to it.
- Contemplation: Individuals recognize the need for change and weigh the pros and cons.
- Preparation: Individuals start planning for change and may take small steps toward it.
- Action: Individuals actively implement the desired change.
- Maintenance: Individuals work to sustain the change and prevent relapse.
The Transtheoretical Model can facilitate behavior change in patients and nursing staff. For patients, nurses can use TTM to develop tailored interventions that promote healthy behaviors, such as smoking cessation or medication adherence. For nursing staff, TTM can guide the implementation of new practices or technologies by addressing each individual's readiness for change and providing appropriate support throughout the change process.
Kotter's Change Theory: A Comprehensive Approach to Change
Kotter's Change Theory, developed by John P. Kotter, is a popular change management model that provides a step-by-step approach for leading and managing organizational change. It comprises eight stages emphasizing the importance of creating a sense of urgency, developing a clear vision, and consolidating gains to ensure lasting change.
The eight stages of Kotter's Change Theory are:
- Establish a sense of urgency.
- Create a guiding coalition.
- Develop a clear vision and strategy.
- Communicate the change vision.
- Empower employees for broad-based action.
- Generate short-term wins.
- Consolidate gains and produce more change.
- Anchor the new approaches in the organizational culture.
If you are familiar with Spradley's change theory, then it will not be difficult for you to understand Kotter's Change Theory. It can be applied in nursing to guide the implementation of large-scale changes within a healthcare setting, such as restructuring a department or adopting a new care delivery model. Following the eight stages, nursing leaders can ensure the change is well-planned, effectively communicated, and embedded into the organization's culture for sustained success.
Lippitt's Change Theory: A Systematic Approach to Change
Lippitt's Change Theory, also known as Lippitt's Phases of Change, is an extension of Lewin's Change Theory that focuses on the role of the change agent in guiding the change process. Developed by Ronald Lippitt, this theory outlines seven steps that provide a systematic approach for planning, implementing, and evaluating change.
Check these Lippitt Change Theory nursing steps:
- Diagnose the problem.
- Assess the motivation and capacity for change.
- Assess the change agent's motivation and resources.
- Establish specific change objectives and strategies.
- Choose the appropriate change agent role.
- Maintain the change through effective communication and involvement.
- Gradually disengage from the change process as the change becomes self-sustaining.
In nursing, Lippitt's Change Theory can be applied to guide nursing professionals in their role as change agents. For example, when implementing a new infection control protocol, nursing leaders can follow the seven steps to diagnose the problem, assess readiness for change, and facilitate the successful implementation of the new practice. This systematic approach ensures a smooth transition and promotes the long-term sustainability of the change.
Examples of Change Theories in Nursing
Implementing a new fall prevention program:.
Nursing leaders can apply Lewin's Change Theory to introduce a new fall prevention program in response to increased patient falls. They would begin by unfreezing the current mindset and practices, introducing evidence-based strategies for fall prevention during the change stage, and refreezing the new practices as part of the standard care routine, ensuring a safer patient environment.
Adopting electronic health records (EHRs):
To improve documentation and communication, hospitals transition from paper records to EHRs. Nursing leaders can utilize Kotter's Change Theory to create a sense of urgency, develop a clear vision, and communicate the new system's benefits to staff. By involving staff in the change process and celebrating short-term wins, they can promote a smooth transition to EHRs.
In conclusion, change theories in nursing play a vital role in understanding, planning, and managing change within the healthcare landscape. By incorporating these theories, nursing professionals can effectively implement and sustain changes that lead to improved patient outcomes and healthcare delivery. Embracing change theories allows nurses to become agents of change and contribute to the ongoing evolution of the nursing profession. And do not forget that our experts at the site can provide further guidance and insights to help you better understand and apply these change theories in your nursing practice.
1. What is the significance of change theory in nursing?
2. what are the types of changes that occur in nursing, 3. what are some strategies for implementing change in nursing, 4. how can resistance to changes be addressed in nursing, 5. how can change in nursing be evaluated.
Ready to proceed? Save 10% your first order

IMAGES
COMMENTS
The Change Theory of Nursing was developed by Kurt Lewin, who is considered the father of social psychology. This theory is his most influential theory. He theorized a three-stage model of change known as unfreezing-change-refreeze model …
The Change Theory of Nursing was developed by Kurt Lewin, who is considered the father of social psychology. This theory is his most influential theory. He theorized a three-stage model of change known as unfreezing-change-refreeze model that requires prior learning to be rejected and replaced.
Sep 18, 2022 · All change initiatives, whether large or small, progress through 3 key stages—pre-change, change, and post-change. Healthcare providers acting as change agents or champions during each stage should align their actions with relevant change theories.
Jun 12, 2023 · Change theory is a structured approach to understanding and managing the process of change in healthcare environments. It equips nurses with the knowledge and skills needed to facilitate smooth transitions and overcome potential barriers when implementing changes in patient care, healthcare policies, and organizational practices.
Aug 9, 2024 · In this, you’ll learn about 10 change management theories in nursing, including best application scenarios, primary sources, and categorization. 1. Lewin’s Change Theory. Primary Source: Lewin, K. (1951). Field theory in social science: Selected theoretical papers. Harper & Brothers.
What is Change Theory in Nursing? Change theory in nursing is a structured approach to understanding, managing, and implementing transformations in healthcare settings. It equips nurses with the knowledge and skills necessary to facilitate smooth transitions and overcome potential barriers when introducing changes in patient care, healthcare ...
Change theory is a middle range nursing theory that guides how healthcare professionals approach, manage, and implement changes in organizations. These theories create a structure for understanding the dynamics of change — how to plan for it, implement it, and ensure that it’s successful.
Jan 22, 2024 · For nurse leaders, the first step in deploying impactful change management within a facility’s nursing team is to have a full understanding of change theory in nursing. Having this understanding can help them interpret the short- and long-term ramifications of each change accurately.
Change is an essential component of nursing practice. Leading change is a challenge for nurse leaders amid the complexities and challenges of evolving health care environments in providing quality patient care.
Aug 3, 2023 · Lewin’s Change Theory stands out as a fundamental framework that has significantly influenced the field of nursing. Developed by psychologist Kurt Lewin in the 1940s, this theory has become a cornerstone for nurses seeking to foster positive change within their organizations.
Sep 16, 2024 · Change theory in nursing refers to concepts and principles that help nurses understand, plan, and implement change in healthcare settings. To provide optimal care, nursing professionals must adapt to new practices, technologies, and patient care standards in an ever-evolving healthcare landscape.