Evidence-based practice improves patient outcomes and healthcare system return on investment: Findings from a scoping review
Affiliations.
- 1 Helene Fuld Health Trust National Institute for Evidence-Based Practice in Nursing & Healthcare, College of Nursing, The Ohio State University, Columbus, Ohio, USA.
- 2 St. John Fisher University, Wegmans School of Nursing, Rochester, New York, USA.
- 3 Sinai Hospital, Baltimore, Maryland, USA.
- 4 Summa Health System, Akron, Ohio, USA.
- 5 The Ohio State University, College of Nursing, Columbus, Ohio, USA.
- 6 Memorial Sloan-Kettering Cancer Center, New York, New York, USA.
- 7 Family CareX, Denver, Colorado, USA.
- 8 Affiliate Faculty, VCU Libraries, Health Sciences Library, Virginia Commonwealth University School of Nursing, Richmond, Virginia, USA.
- PMID: 36751881
- DOI: 10.1111/wvn.12621
Background: Evidence-based practice and decision-making have been consistently linked to improved quality of care, patient safety, and many positive clinical outcomes in isolated reports throughout the literature. However, a comprehensive summary and review of the extent and type of evidence-based practices (EBPs) and their associated outcomes across clinical settings are lacking.
Aims: The purpose of this scoping review was to provide a thorough summary of published literature on the implementation of EBPs on patient outcomes in healthcare settings.
Methods: A comprehensive librarian-assisted search was done with three databases, and two reviewers independently performed title/abstract and full-text reviews within a systematic review software system. Extraction was performed by the eight review team members.
Results: Of 8537 articles included in the review, 636 (7.5%) met the inclusion criteria. Most articles (63.3%) were published in the United States, and 90% took place in the acute care setting. There was substantial heterogeneity in project definitions, designs, and outcomes. Various EBPs were implemented, with just over a third including some aspect of infection prevention, and most (91.2%) linked to reimbursement. Only 19% measured return on investment (ROI); 94% showed a positive ROI, and none showed a negative ROI. The two most reported outcomes were length of stay (15%), followed by mortality (12%).
Linking evidence to action: Findings indicate that EBPs improve patient outcomes and ROI for healthcare systems. Coordinated and consistent use of established nomenclature and methods to evaluate EBP and patient outcomes are needed to effectively increase the growth and impact of EBP across care settings. Leaders, clinicians, publishers, and educators all have a professional responsibility related to improving the current state of EBP. Several key actions are needed to mitigate confusion around EBP and to help clinicians understand the differences between quality improvement, implementation science, EBP, and research.
Keywords: evidence-based decision making; evidence-based practice; healthcare; patient outcomes; patient safety; return on investment.
© 2023 The Authors. Worldviews on Evidence-based Nursing published by Wiley Periodicals LLC on behalf of Sigma Theta Tau International.

Publication types
- Systematic Review
- Delivery of Health Care*
- Evidence-Based Practice* / methods
- Quality Improvement
An official website of the United States government
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Publications
- Account settings
- Advanced Search
- Journal List
Total quality management in the health-care context: integrating the literature and directing future research
Majdi m alzoubi, zm al-hamdan.
- Author information
- Article notes
- Copyright and License information
Correspondence: KS HayatiDepartment of Community Health, Faculty of Medicine and Health Sciences, University Putra Malaysia, UPM Serdang, Selangor Darul Ehsan, 43400, MalaysiaEmail [email protected]
Received 2018 Dec 4; Accepted 2019 Jul 11; Collection date 2019.
This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution – Non Commercial (unported, v3.0) License ( http://creativecommons.org/licenses/by-nc/3.0/ ). By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms ( https://www.dovepress.com/terms.php ).
Synergistic integration of predictors and elements that determine the success of total quality management (TQM) implementations in hospitals has been the bane of theoretical development in the TQM research area. Thus, this paper aims to offer a systematic literature review to provide a foundation on which research on TQM can be built and to identify the predictors of successful TQM in the health-care context.
Materials and methods
A systematic literature survey was adopted in this paper, involving the review of 25 relevant researched articles found in the databases Science Direct, EBSCO, MEDLINE, CINAHL and PubMed.
The systematic literature survey reveals five variables to be core predictors of TQM, signifying how important these variables are in the successful implementation of TQM in the health-care context. Also, it is revealed that the identified core predictors have positive effects on an improved health-care system. However, the systematic survey of the literature reveals a dearth of studies on TQM in the health-care context.
As TQM has become an important management approach for advancing effectiveness in the health-care sector, this kind of research is of value to researchers and managers. Stakeholders in the health sectors should introduce and implement TQM in hospitals and clinics. Nevertheless, this study has limitations, including that the databases and search engines adopted for the literature search are not exhaustive.
Keywords: total quality management, total quality management implementation, health care, commitment, systematic literature review, critical success factors
Introduction
Given the snowballing global economic competition and other external pressures, organizations have been compelled to pursue enduring quality and quality management which will, in turn, enhance their competitive advantage. Quality as a concept has metamorphosed over the years, and it involves objective quality bordering on the characteristics and quality of goods and services that meet implicit and explicit customer demands. It also includes subjective quality which denotes the capability to produce goods and services in the best, effective and efficient manner. 1
Looking at the health-care context, quality has always been aimed at since the time of Florence Nightingale. 2 Given that quality assurance is a requisite for economic survival, 3 and that it is an ethical, legal and social rights matter, 4 the health sector has been worried about it for more than a decade .2 Quality assurance is significant as it concerns customer satisfaction and the reduction of risks connected with health care to a minimum. 5 In the present time, health care has become a developing profession with an approach to care quality via the appraisal and regulation of structure, process and care result components. 6
Given the ever-increasing competitive and dynamic environment in which hospitals operate, and the need to augment hospitals’ performance and health-care quality, researchers 2 , 7 – 9 have conducted considerable research on enhancement of health-care quality. Moreover, given that nurse performance is crucial to the overall performance of the hospital and effective health-care system, there has been a research focus on nurse performance. 7 Nurses represent a large percentage of the health workers in any hospital. Nurses would play a significant role in the implementation of any intervention programs introduced by any hospital.
Moreover, research 8 – 11 has shown that the health-care system is facing a myriad of challenges which include high care cost, swiftly increasing dependence on technology, economic pressure on health organizations, reduction in health-care quality, 8 , 10 fulfillment of patients’ needs, 9 augmented numbers of patients who are suffering from multiple illnesses, increased demand for high-quality care, increased health-care costs and cost-containment pressures (Organization for Economic Cooperation and Development [OECD] 2007). 11 Some studies have indicated that an active way of surmounting health-care challenges is through an intervention program that will border on quality management (eg, total quality management [TQM]). 12
TQM is a system implemented by the management of an organization to achieve the satisfaction of customers/patients .13 The importance of TQM as a strategy to improve organizational performance has grown in this era of globalization. 14 Numerous research has revealed the role of TQM in the enrichment of system quality and enhancement of both employee and organizational performance. TQM is known for continuous quality improvement, quality management and total quality control. 10 TQM is held to be an innovative approach to the management of organizations. In the medical sector, TQM integrates quality orientation in all processes and procedures in health-care delivery .15 It is now being widely adopted in the medical sector of many countries. The research by Vituri and Évora 2 indicates that the literature on TQM in health sectors reveals that TQM has been fully adopted in some health institutions.
The implementation of TQM, upon which the success of TQM hinges, is intricate and complex; it depends on a good combination of certain predictors (ie, critical success factors [CSF]), and its benefits are difficult to accomplish .16 Different means of integrating predictors of TQM, although inconsistent, have emerged in the literature. 17 Some predictors have been considered crucial to TQM success, 18 and thus the exceptional predictors which can be adopted by organizations, irrespective of their industry, type, size or location. 19 These predictors are regarded as the determinants of firm performance via effective implementation of TQM.
Nevertheless, synergistic integration of predictors and elements, otherwise known as CSFs and which determine the success of TQM implementation, has been the bane of theoretical development in the TQM research area. Some of these predictors have been reported, by extant studies, 20 to have a positive impact on performance.
Likewise, substantive problems exist and can hamper theoretical development in the research area. The literature lacks foundation and structure on which the research on TQM in the health-care context is based, and connections between studies on TQM in the health-care context can hardly be drawn. The current state of extant research on TQM in the health-care context indicates that there is a need for more research in the area. 21 New knowledge development regarding identification of fitting predictors for successful TQM that enhance effectiveness in the health-care sector should be developed and where further research needs to be done should be identified.
Considering the extant works on a systematic literature review on predictors of TQM, two English written studies 14 , 22 are discernible, but Hietschold et al 14 focused on CSFs of TQM in general contexts while Aquilani et al 22 focused on the identification of TQM research, implementation of TQM research and impact-of-TQM-on-performance research in general contexts. Besides these two studies, no studies have focused on the systematic literature survey of predictors/elements of TQM in the health-care context.
Therefore, undertaking a systematic literature review in this aspect of research is germane, and this paper is poised to do as such. This paper conducts a systematic literature survey to provide a foundation stone on which research on TQM in the health-care context can be built, to evaluate the current state of evidence for TQM in the health-care context, to reveal inadequacies in the literature and to point to where further research needs to be done.
This research is guided by the following research question: what are the predictors of successful TQM in the health-care context between the period of 2005 and 2016? Like the two previous studies on a systematic literature review of TQM, this paper adopts and applies the three core steps of planning, execution and reporting that constitute a systematic literature survey. 23
This research seeks to obtain the most important predictors of successful TQM in the health-care context. This includes the review of published peer-reviewed works in English-language journals, which were published between 2005 and 2016. The literature was sourced from Science Direct, EBSCO, MEDLINE (Medical Literature Analysis and Retrieval System Online), CINAHL (Cumulative Index of Nursing and Allied Health Literature) and PubMed (US National Library of Medicine).
As part of the process of systematic literature analysis in this paper, a structured search of the academic literature was conducted to find published articles that identified TQM, total quality management, implementation, CSFs, health care and nursing. The keywords used in the search are TQM, total quality management, implementation, critical success factors, health care and nursing.
As presented in Figure 1 , a search of Science Direct, MEDLINE, EBSCO, CINAHL and PubMed yielded 2133, 6341, 1867, 7 and 474 articles, respectively. Then, repeated citations, dissertations and case studies were deleted. Via reading of the title and abstract, the remaining articles were narrowed down by relevance. Only peer-reviewed academic and practice articles that focus on total quality management, implementation, CSFs health care and nursing were selected. This exercise yielded a total of 475 articles which were published between 2005 and 2016.
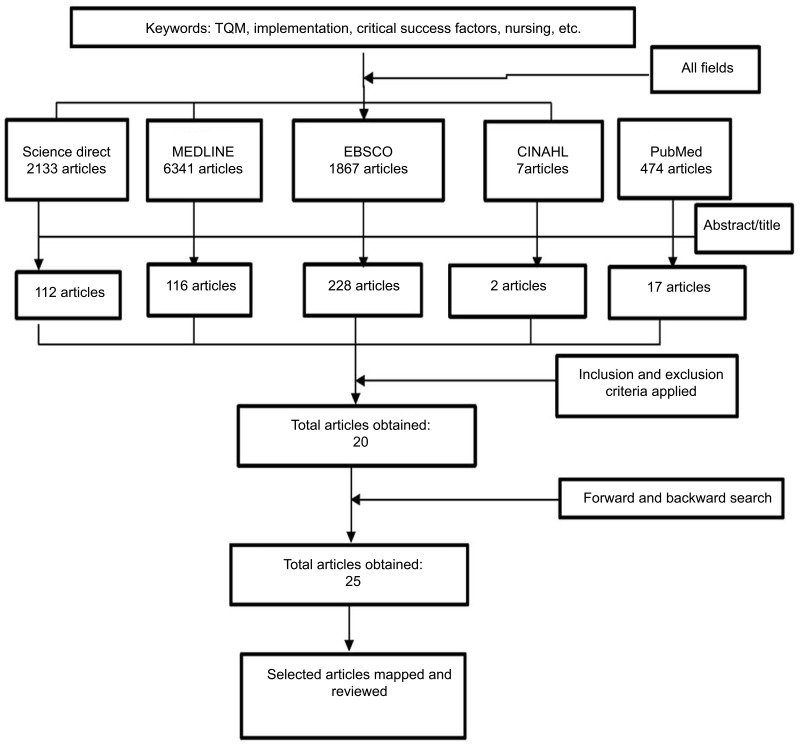
Consort flow chart of systematic review method.
Abbreviation: TQM, total quality management.
Furthermore, inclusion and exclusion criteria were applied to narrow down the yielded articles. The inclusion criteria involved articles which were written in English language and published between 2005 and 2016, articles that dwell on implementation and critical factors clearly, articles from any geographical location which examined TQM, TQM principles, TQM tools and methods in the context of the health-care sector, and TQM studies that used a quantitative research approach and quasi-experimental research design. The exclusion criteria involved articles which are written in non-English language and published before 2005 or after 2016, studies in which the population and sample were not health-care workers practicing inside hospitals, gray literature or works that are not published in a peer-reviewed journal, dissertations/theses, proceedings, published abstracts, studies with qualitative research methods, and commentary articles written to convey opinion or stimulate research or discussion, with no research component. By employing these inclusion and exclusion criteria, 20 articles were generated. Moreover, to guarantee all-inclusiveness and to widen the scope of the review, a forward and backward search of citations in articles was conducted. This was recognized via the database searches, and 25 articles were finally selected. Thereafter, the 25 generated articles were fully perused.
Likewise, for exhaustive research, the approach adopted in this paper also involved the identification and measurement of predictors (CSFs) of TQM. This was done by identifying the most common or important predictors in the selected 25 works that analyze the existing models and/or scales in other contexts, industries or countries. It also includes recognition of the papers that investigate the influence of TQM implementation and/or the impact of predictors of TQM on performance. Additionally, for a proper review of the selected works, adequate plotting of the development of the line of reasoning, integrating and synthesizing the studies, authors, study design, study population, variables, measures of variables and findings of each selected article were identified and noted down. Figure 1 represents the consort flow chart of the systematic review method.
Findings and discussion
Altogether, 25 researched articles were eventually reviewed. All of the selected 25 articles are based on empirical evidence, although a possible limitation of this systematic review strategy might be the exclusion of qualitative studies in the research. Based on Table 1 , five predictors were identified. These are presented in Table 2 .
Matrix of the reviewed literature
Abbreviations: HR, human resources; TQM, total quality management.
TQM predictors in the reviewed studies
The researched literature on predictors of successful TQM implementation was found to be from various countries but in the same health sector. While some predictors adopted by a few of the researched studies were identified, the most frequent and core predictors were identified and considered. As depicted in Table 2 , education and training, continuous quality improvement, patient focus/satisfaction, top management commitment and teamwork appear to be the core predictors (CSFs) in this review. This finding validates how important these variables are in the successful implementation of TQM in the health-care context.
It is noteworthy that the core predictors (ie, education and training, continuous quality improvement, patient focus/satisfaction, top management commitment and teamwork) identified in this study were among the variables found to be central and frequently used CSFs in the previous systematic-review-based studies. 14 , 21 This validates and confirms the findings of the previous studies.
Moreover, it is found that the most adopted research method in TQM in the health-care context is cross-sectional research; 56% of the reviewed researched articles 41 – 46 used a cross-sectional research design, but 32% of the studies employed a quasi-experimental research approach. This indicates that there is still a need for more research on TQM in the health-care context which will adopt a quasi-experimental research approach, because quasi-experimental research design can be very useful in recognizing general trends from the results, and reduces the difficulty and ethical worries that may be connected with the pre-selection and random assignment of test subjects. On the geographical location aspect, the result of this analysis showed that 28% of the reviewed studies were conducted in Iran while 20% of the reviewed studies were conducted in Jordan; 12% and 8% of the reviewed studies were conducted in Saudi Arabia and Pakistan, respectively. The other studies, 4% each, came from India, Namibia, Turkey, the United States, France and Mauritius.
With regards to the influence of predictors on performance in the researched studies, it is found that all of the selected articles 47 , 48 , 49 , 50 ,. 51 that examined the effects of the core predictors (continuous quality improvement, education and training, patient focus/satisfaction, top management commitment and teamwork) of TQM indicate a positive effect of TQM in the health-care sector.
More so, the findings of this review signify that predictors of TQM implementation will result in higher levels of nurse performance .51 In addition, the literature and empirical evidence have shown that TQM in an organizational process always results in better performance of the organization. TQM focuses on patient satisfaction, organization problem identification, building and promotion of open decision-making among employees. It embraces a holistic strategy that gives room for every worker to share responsibility for the quality of the work done. It makes use of analytical mechanisms, such as flow and statistical charts and checksheets, to gather information about activities in an organization. 52 In the medical sector, TQM aims at embedding orientation of quality in all processes and procedures in the delivery of health services .15
Nevertheless, this literature survey is not an exhaustive review of the literature on TQM as it solely focused on the effect of TQM. Future research should widen the scope of this paper by including studies conducted in other contexts (eg, education, manufacturing, etc) and studies that use different research methods (eg, longitudinal research method, randomized control trial method). While TQM predictors have increased in number to reach a total of 59 TQM practices, 21 TQM predictors in the context of health care are few but growing. Investigating the nature of TQM predictors and the methods used in examining them indicates that researchers may have been keen in searching for new predictors instead of trying to cluster them and identify those that are critical for successful TQM implementation. In addition, research on TQM predictors in the health-care sector is scanty, as noted previously.
Practically, given the identified core TQM predictors in this study, it is evident that hospitals’ management should consider entrenchment of continuous quality improvement, education and training, patient focus/satisfaction top management commitment and teamwork in the implementation of TQM, which will consequently enhance hospital performance. Given that TQM predictors are many and some of them have been considered core in several specific contexts, industries, dimensions, etc, it is held that stakeholders in different sectors/industries should begin to identify the most vital TQM practices that suit their situations, goals, strategies and expected performances.
Conclusion and recommendations
As TQM has become an important management approach for advancing performance, this kind of research is of value to researchers and managers. Nevertheless, this study has limitations, including that the databases and search engines adopted for the literature search are not exhaustive. Although a good number of keywords are used, there can be other likely keywords that can be included.
This work has contributed to the enrichment of the relevant literature and made theoretical and methodological contributions. It has provided a foundation on which research on TQM can be built via review of the work done between 2005 and 2016, plotting the development of the line of reasoning, and integration and synthesis of studies from TQM in the health-care context. It has also contributed by evaluating the current state of evidence regarding TQM, indicating inadequacies in the literature and pointing to where further research needs to be done. Thus, it contributes to the present body of knowledge as well as the research on TQM in the health-care context.
This work has also established that the most adopted research method in health-care-based TQM is cross-sectional research, followed by quasi-experimental research, and the researched studies were mostly conducted in Asia. The findings of the researched literature indicate a positive effect of TQM in the health-care context, indicating that TQM implementation, which contains the identified core predictors, will result in higher levels of performance. Furthermore, TQM implementation can help health-care professionals to gain more qualified behaviors with total commitment to work toward handling the patients, which in the long run will augment their performance.
The findings of the reviewed studies indicate how it would be useful for stakeholders in the health sectors to introduce and implement TQM in the hospitals and clinics, as this would enhance the performance of the health workers and consequently improve organizational performance. Given the limitations of this work, it is sufficed to suggest that future research should widen the scope of this paper by including studies conducted in other contexts and studies that use different research methods, and it should also develop a comprehensive TQM taxonomy to explain how and why TQM practices coalesce within systems that facilitate higher performance.
The authors report no conflicts of interest in this work.
- 1. Bonechi L, Carmignani G, Mirandola R. La Gestione Della Qualità Nelle Organizzazioni-dalla Conformità All’eccellenza Gestionale . Edizioni Plus srl; 2004. [ Google Scholar ]
- 2. Vituri DW, Évora YDM. Total Quality Management and hospital nursing: an integrative literature review. Rev Bras Enferm . 2015;68(5):945–952. doi: 10.1590/0034-7167.2015680525i [ DOI ] [ Google Scholar ]
- 3. Antunes M, Sfakiotakis E. Effect of high temperature stress on ethylene biosynthesis, respiration and ripening of ‘Hayward’kiwifruit. Postharvest Biol Technol . 2000;20(3):251–259. doi: 10.1016/S0925-5214(00)00136-8 [ DOI ] [ Google Scholar ]
- 4. Adami C, Ofria C, Collier TC. Evolution of biological complexity. Proc Natl Acad Sci . 2000;97(9):4463–4468. doi: 10.1073/pnas.97.9.4463 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 5. Padilha KG. Iatrogenic occurrences and the quality focus. Rev Lat Am Enfermagem . 2001;9(5):91–96. doi: 10.1590/s0104-11692001000500014 [ DOI ] [ PubMed ] [ Google Scholar ]
- 6. Haddad M, Évora YDM. Qualidade da assistência de enfermagem: a opinião do paciente internado em hospital universitário público. Ciênc Cuid Saúde . 2008;7:45–52. doi: 10.4025/cienccuidsaude.v7i0.6559 [ DOI ] [ Google Scholar ]
- 7. Wright TA, Bonett DG. The moderating effects of employee tenure on the relation between organizational commitment and job performance: a meta-analysis. J Appl Psychol . 2002;87(6):1183. doi: 10.1037/0021-9010.87.6.1183 [ DOI ] [ PubMed ] [ Google Scholar ]
- 8. Aiken LH, Sermeus W, Van Den Heede K, et al. Patient safety, satisfaction, and quality of hospital care: cross sectional surveys of nurses and patients in 12 countries in Europe and the United States. BMJ . 2012;344:e1717. doi: 10.1136/bmj.e1717 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 9. Chang C-S, Chen S-Y, Lan Y-T. Service quality, trust, and patient satisfaction in interpersonal-based medical service encounters. BMC Health Serv Res . 2013;13(1):22. doi: 10.1186/1472-6963-13-438 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 10. McClellan M, Rivlin A. Improving Health while Reducing Cost Growth: What is Possible . Engelberg Center for Health Care Reform at Brookings; 2014. [ Google Scholar ]
- 11. World Health Organization. The World Health Report 2000: Health Systems: Improving Performance . World Health Organization; 2000. [ Google Scholar ]
- 12. Cummings TG, Worley CG. Organization Development and Change . Cengage learning; 2014. [ Google Scholar ]
- 13. Srima S, Wannapiroon P, Nilsook PJP-S, Sciences B. Design of total quality management information system (TQMIS) for model school on best practice. 2015;174:2160–2165. [ Google Scholar ]
- 14. Hietschold N, Reinhardt R, Gurtner S. Measuring critical success factors of TQM implementation successfully–a systematic literature review. Int J Prod Res . 2014;52(21):6254–6272. doi: 10.1080/00207543.2014.918288 [ DOI ] [ Google Scholar ]
- 15. MoHSW T. Implementation Guidelines for 5S-KAIZEN-TQM Approaches in Tanzania . Dar es Salaam (Tanzania): Ministry of Health and Social Welfare; 2013. [ Google Scholar ]
- 16. Mohammad Mosadegh Rad A. The impact of organizational culture on the successful implementation of total quality management. TQM Magazine . 2006;18(6):606–625. doi: 10.1108/09544780610707101 [ DOI ] [ Google Scholar ]
- 17. Ismail Salaheldin S. Critical success factors for TQM implementation and their impact on performance of SMEs. Int J Prod Perform Manage . 2009;58(3):215–237. doi: 10.1108/17410400910938832 [ DOI ] [ Google Scholar ]
- 18. Kumar S, Ghildayal NS, Shah RN. Examining quality and efficiency of the US healthcare system. Int J Health Care Qual Assur . 2011;24(5):366–388. doi: 10.1108/09526861111139197 [ DOI ] [ PubMed ] [ Google Scholar ]
- 19. Zairi M, Alsughayir AA. The adoption of excellence models through cultural and social adaptations: an empirical study of critical success factors and a proposed model. Total Qual Manage Bus Excellence . 2011;22(6):641–654. doi: 10.1080/14783363.2011.580654 [ DOI ] [ Google Scholar ]
- 20. Sadikoglu E, Olcay H. The effects of total quality management practices on performance and the reasons of and the barriers to TQM practices in Turkey. Adv Decis Sci . 2014;2014:1–17. doi: 10.1155/2014/537605 [ DOI ] [ Google Scholar ]
- 21. Aquilani B, Silvestri C, Ruggieri A, Gatti C. A systematic literature review on total quality management critical success factors and the identification of new avenues of research. Tqm J . 2017;29(1):184–213. doi: 10.1108/TQM-01-2016-0003 [ DOI ] [ Google Scholar ]
- 22. Aquilani B, Silvestri C, Ioppolo G, Ruggieri A. The challenging transition to bio-economies: Towards a new framework integrating corporate sustainability and value co-creation. J Clean Prod . 2018;172:4001–4009. doi: 10.1016/j.jclepro.2017.03.153 [ DOI ] [ Google Scholar ]
- 23. Tranfield D, Denyer D, Smart P. Towards a methodology for developing evidence‐informed management knowledge by means of systematic review. Br J Manage . 2003;14(3):207–222. doi: 10.1111/bjom.2003.14.issue-3 [ DOI ] [ Google Scholar ]
- 24. Irfan S, Ijaz A, Kee D, Awan M. Improving operational performance of public hospital in Pakistan: A TQM based approach. World Appl Sci J . 2012;19(6):904–913. [ Google Scholar ]
- 25. Mrayyan MT, Al‐Faouri I. Predictors of career commitment and job performance of Jordanian nurses. J Nurs Manag . 2008;16(3):246–256. doi: 10.1111/j.1365-2834.2007.00797.x [ DOI ] [ PubMed ] [ Google Scholar ]
- 26. Danial Z. Effect of Total Quality Management in Determining the Educational Needs of Critical Wards Nurses . 2009. [ Google Scholar ]
- 27. Awases MH, Bezuidenhout MC, Roos JH. Factors affecting the performance of professional nurses in Namibia. Curationis . 2013;36(1):1–8. doi: 10.4102/curationis.v36i1.108 [ DOI ] [ PubMed ] [ Google Scholar ]
- 28. Al-Ahmadi H. Factors affecting performance of hospital nurses in Riyadh Region, Saudi Arabia. Int J Health Care Qual Assur . 2009;22(1):40–54. doi: 10.1108/09526860910927943 [ DOI ] [ PubMed ] [ Google Scholar ]
- 29. Kim K, Han Y, Kwak Y, Kim J-S. Professional quality of life and clinical competencies among Korean nurses. Asian Nurs Res . 2015;9(3):200–206. doi: 10.1016/j.anr.2015.03.002 [ DOI ] [ PubMed ] [ Google Scholar ]
- 30. AbuAlRub RF, AL‐ZARU IM. Job stress, recognition, job performance and intention to stay at work among Jordanian hospital nurses. J Nurs Manag . 2008;16(3):227–236. doi: 10.1111/j.1365-2834.2007.00810.x [ DOI ] [ PubMed ] [ Google Scholar ]
- 31. Güleryüz G, Güney S, Aydın EM, Aşan Ö. The mediating effect of job satisfaction between emotional intelligence and organisational commitment of nurses: a questionnaire survey. Int J Nurs Stud . 2008;45(11):1625–1635. doi: 10.1016/j.ijnurstu.2008.02.004 [ DOI ] [ PubMed ] [ Google Scholar ]
- 32. Lashgari MH, Arefanian S, Mohammadshahi A, Khoshdel AR. Effects of the total quality management implication on patient satisfaction in the Emergency Department of Military Hospitals. J Arch Mil Med . 2015;3(1). doi: 10.5812/jamm [ DOI ] [ Google Scholar ]
- 33. Navipour H, Nayeri ND, Hooshmand A, Zargar MT. An investigation into the effects of quality improvement method on patients’ satisfaction: a semi experimental research in Iran. Acta Med Iran . 2011;49(1):38–43. [ PubMed ] [ Google Scholar ]
- 34. Mosadeghrad AM. Developing and validating a total quality management model for healthcare organisations. TQM J . 2015;27(5):544–564. doi: 10.1108/TQM-04-2013-0051 [ DOI ] [ Google Scholar ]
- 35. Mohammad Mosadeghrad A. Why TQM does not work in Iranian healthcare organisations. Int J Health Care Qual Assur . 2014;27(4):320–335. doi: 10.1108/IJHCQA-11-2012-0110 [ DOI ] [ PubMed ] [ Google Scholar ]
- 36. Mosadeghrad AM. Implementing strategic collaborative quality management in healthcare sector. Int J Strat Change Manage . 2012;4(3/4):203–228. doi: 10.1504/IJSCM.2012.051846 [ DOI ] [ Google Scholar ]
- 37. Jones KJ, Skinner AM, High R, Reiter-Palmon R. A theory-driven, longitudinal evaluation of the impact of team training on safety culture in 24 hospitals. BMJ Qual Saf . 2013;22(5):394–404. doi: 10.1136/bmjqs-2012-000939 [ DOI ] [ PubMed ] [ Google Scholar ]
- 38. Ullah JH, Ahmed R, Malik JI, Khan MA. Outcome of 7-S, TQM technique for healthcare waste management. J Coll Physicians Surg Pak . 2011;21(12):731–734. doi: 12.2011/JCPSP.731734 [ PubMed ] [ Google Scholar ]
- 39. Padma P, Rajendran C, Sai Lokachari P. Service quality and its impact on customer satisfaction in Indian hospitals: Perspectives of patients and their attendants. Benchmarking . 2010;17(6):807–841. doi: 10.1108/14635771011089746 [ DOI ] [ Google Scholar ]
- 40. Ramseook-Munhurrun P, Munhurrun V, Panchoo A. Total Quality Management Adoption in a Public Hospital: Evidence from Mauritius . 2011. [ Google Scholar ]
- 41. Alaraki MS. The impact of critical total quality management practices on hospital performance in the ministry of health hospitals in Saudi Arabia. Qual Manage Healthcare . 2014;23(1):59–63. doi: 10.1097/QMH.0000000000000018 [ DOI ] [ PubMed ] [ Google Scholar ]
- 42. Al-Shdaifat EA. Implementation of total quality management in hospitals. J Taibah Univ Med Sci . 2015;10(4):461–466. doi: 10.1016/j.jtumed.2015.05.004 [ DOI ] [ Google Scholar ]
- 43. Larber M, Savis S. Factors affecting nurses organizational commitment. Obzornik Zdravstvene Nege . 2014;48(4):294–301. [ Google Scholar ]
- 44. Duggirala M, Rajendran C, Anantharaman R. Patient-perceived dimensions of total quality service in healthcare. Benchmarking . 2008;15(5):560–583. doi: 10.1108/14635770810903150 [ DOI ] [ Google Scholar ]
- 45. Naser Alolayyan M, Anuar Mohd Ali K, Idris F. The influence of total quality management (TQM) on operational flexibility in Jordanian hospitals: medical workers’ perspectives. Asian J Qual . 2011;12(2):204–222. doi: 10.1108/15982681111158751 [ DOI ] [ Google Scholar ]
- 46. Sweis RJ, Al-Mansour A, Tarawneh M, Al-Dweik G. The impact of total quality management practices on employee empowerment in the healthcare sector in Saudi Arabia: a study of King Khalid Hospital. Int J Prod Qual Manage . 2013;12(3):271–286. doi: 10.1504/IJPQM.2013.056149 [ DOI ] [ Google Scholar ]
- 47. Kumar R, Somrongthong R, Ahmed J. Impact of waste management training intervention on knowledge, attitude and practices of teaching hospital workers in Pakistan. Pak J Med Sci . 2016;32(3):705. doi: 10.12669/pjms.323.9903 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 48. Sagy M. Optimizing patient care processes in a children’s hospital using Six Sigma. JCOM . 2009;16:9. [ Google Scholar ]
- 49. Denker AG. Transformational Leadership in Nursing: A Pilot Nurse Leader Development Program . 2014. [ Google Scholar ]
- 50. François P, Vinck D, Labarère J, Reverdy T, Peyrin J-C. Assessment of an intervention to train teaching hospital care providers in quality management. BMJ Qual Saf . 2005;14(4):234–239. doi: 10.1136/qshc.2004.011924 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 51. El-Tohamy AE-MA, Al Raoush AT. The impact of applying total quality management principles on the overall hospital effectiveness: an empirical study on the HCAC accredited governmental hospitals in Jordan. Eur Sci J . 2015;11(10). [ Google Scholar ]
- 52. Kaluzny AD, McLaughlin CP, Simpson K. Applying total quality management concepts to public health organizations. Public Health Rep . 1992;107(3):257. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- View on publisher site
- PDF (446.8 KB)
- Collections
Similar articles
Cited by other articles, links to ncbi databases.
- Download .nbib .nbib
- Format: AMA APA MLA NLM
Add to Collections
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Busse R, Klazinga N, Panteli D, et al., editors. Improving healthcare quality in Europe: Characteristics, effectiveness and implementation of different strategies [Internet]. Copenhagen (Denmark): European Observatory on Health Systems and Policies; 2019. (Health Policy Series, No. 53.)

Improving healthcare quality in Europe: Characteristics, effectiveness and implementation of different strategies [Internet].
3 measuring healthcare quality.
Wilm Quentin , Veli-Matti Partanen , Ian Brownwood , and Niek Klazinga .
3.1. Introduction
The field of quality measurement in healthcare has developed considerably in the past few decades and has attracted growing interest among researchers, policy-makers and the general public (Papanicolas & Smith, 2013 ; EC, 2016 ; OECD, 2019 ). Researchers and policy-makers are increasingly seeking to develop more systematic ways of measuring and benchmarking quality of care of different providers. Quality of care is now systematically reported as part of overall health system performance reports in many countries, including Australia, Belgium, Canada, Italy, Mexico, Spain, the Netherlands, and most Nordic countries. At the same time, international efforts in comparing and benchmarking quality of care across countries are mounting. The Organisation for Economic Co-operation and Development (OECD) and the EU Commission have both expanded their efforts at assessing and comparing healthcare quality internationally (Carinci et al., 2015 ; EC, 2016 ). Furthermore, a growing focus on value-based healthcare (Porter, 2010 ) has sparked renewed interest in the standardization of measurement of outcomes (ICHOM, 2019 ), and notably the measurement of patient-reported outcomes has gained momentum (OECD, 2019 ).
The increasing interest in quality measurement has been accompanied and supported by the growing ability to measure and analyse quality of care, driven, amongst others, by significant changes in information technology and associated advances in measurement methodology. National policy-makers recognize that without measurement it is difficult to assure high quality of service provision in a country, as it is impossible to identify good and bad providers or good and bad practitioners without reliable information about quality of care. Measuring quality of care is important for a range of different stakeholders within healthcare systems, and it builds the basis for numerous quality assurance and improvement strategies discussed in Part II of this book. In particular, accreditation and certification ( see Chapter 8 ), audit and feedback ( see Chapter 10 ), public reporting ( see Chapter 13 ) and pay for quality ( see Chapter 14 ) rely heavily on the availability of reliable information about the quality of care provided by different providers and/or professionals. Common to all strategies in Part II is that without robust measurement of quality, it is impossible to determine the extent to which new regulations or quality improvement interventions actually work and improve quality as expected, or if there are also adverse effects related to these changes.
This chapter presents different approaches, frameworks and data sources used in quality measurement as well as methodological challenges, such as risk-adjustment, that need to be considered when making inferences about quality measures. In line with the focus of this book ( see Chapter 1 ), the chapter focuses on measuring quality of healthcare services, i.e. on the quality dimensions of effectiveness, patient safety and patient-centredness. Other dimensions of health system performance, such as accessibility and efficiency, are not covered in this chapter as they are the focus of other volumes about health system performance assessment ( see , for example, Smith et al., 2009 ; Papanicolas & Smith, 2013 ; Cylus, Papanicolas & Smith, 2016 ). The chapter also provides examples of quality measurement systems in place in different countries. An overview of the history of quality measurement (with a focus on the United States) is given in Marjoua & Bozic ( 2012 ). Overviews of measurement challenges related to international comparisons are provided by Forde, Morgan & Klazinga ( 2013 ) and Papanicolas & Smith ( 2013 ).
3.2. How can quality be measured? From a concept of quality to quality indicators
Most quality measurement initiatives are concerned with the development and assessment of quality indicators (Lawrence & Olesen, 1997 ; Mainz, 2003 ; EC, 2016 ). Therefore, it is useful to step back and reflect on the idea of an indicator more generally. In the social sciences, an indicator is defined as “a quantitative measure that provides information about a variable that is difficult to measure directly” (Calhoun, 2002 ). Obviously, quality of care is difficult to measure directly because it is a theoretical concept that can encompass different aspects depending on the exact definition and the context of measurement.
Chapter 1 has defined quality of care as “the degree to which health services for individuals and populations are effective, safe and people-centred”. However, the chapter also highlighted that there is considerable confusion about the concept of quality because different institutions and people often mean different things when using it. To a certain degree, this is inevitable and even desirable because quality of care does mean different things in different contexts. However, this context dependency also makes clarity about the exact conceptualization of quality in a particular setting particularly important, before measurement can be initiated.
In line with the definition of quality in this book, quality indicators are defined as quantitative measures that provide information about the effectiveness, safety and/or people-centredness of care. Of course, numerous other definitions of quality indicators are possible (Mainz, 2003 ; Lawrence & Olesen, 1997 ). In addition, some institutions, such as the National Quality Forum (NQF) in the USA, use the term quality measure instead of quality indicator . Other institutions, such as the NHS Indicator Methodology and Assurance Service and the German Institute for Quality Assurance and Transparency in Health Care (IQTIG), define further attributes of quality indicators (IQTIG, 2018 ; NHS Digital, 2019a ). According to these definitions, quality indicators should provide:
- a quality goal, i.e. a clear statement about the intended goal or objective, for example, inpatient mortality of patients admitted with pneumonia should be as low as possible;
- a measurement concept, i.e. a specified method for data collection and calculation of the indicator, for example, the proportion of inpatients with a primary diagnosis of pneumonia who died during the inpatient stay; and
- an appraisal concept, i.e. a description of how a measure is expected to be used to judge quality, for example, if inpatient mortality is below 10%, this is considered to be good quality.
Often the terms measures and indicators are used interchangeably. However, it makes sense to reserve the term quality indicator for measures that are accompanied by an appraisal concept (IQTIG, 2018 ). This is because measures without an appraisal concept are unable to indicate whether measured values represent good or bad quality of care. For example, the readmission rate is a measure for the number of readmissions. However, it becomes a quality indicator if a threshold is defined that indicates “higher than normal” readmissions, which could, in turn, indicate poor quality of care. Another term that is frequently used interchangeably with quali ty indicator , in particular in the USA, is quality metric . However, a quality metric also does not necessarily define an appraisal concept, which could potentially distinguish it from an indicator. At the same time, the term qua l ity metric is sometimes used more broadly for an entire system that aims to evaluate quality of care using a range of indicators.
Operationalizing the theoretical concept of quality by translating it into a set of quality indicators requires a clear understanding of the purpose and context of measurement. Chapter 2 has introduced a five-lens framework for describing and classifying quality strategies. Several of these lenses are also useful for better understanding the different aspects and contexts that need to be taken into account when measuring healthcare quality. First, it is clear that different indicators are needed to assess the three dimensions of quality, i.e. effectiveness, safety and/or patient-centredness, because they relate to very different concepts, such as patient health, medical errors and patient satisfaction.
Secondly, quality measurement has to differ depending on the concerned function of the healthcare system, i.e. depending on whether one is aiming to measure quality in preventive, acute, chronic or palliative care. For example, changes in health outcomes due to preventive care will often be measurable only after a long time has elapsed, while they will be visible more quickly in the area of acute care. Thirdly, quality measurement will vary depending on the target of the quality measurement initiative, i.e. payers, provider organizations, professionals, technologies and/or patients. For example, in some contexts it might be useful to assess the quality of care received by all patients covered by different payer organizations (for example, different health insurers or regions) but more frequently quality measurement will focus on care provided by different provider organizations. In international comparisons, entire countries will constitute another level or target of measurement.
In addition, operationalizing quality for measurement will always require a focus on a limited set of quality aspects for a particular group of patients. For example, quality measurement may focus on patients with hip fracture treated in hospitals and define aspects of care that are related to effectiveness (for example, surgery performed within 24 hours of admission), safety (for example, anticoagulation to prevent thromboembolism), and/or patient-centredness of care (for example, patient was offered choice of spinal or general anaesthesia) (Voeten et al., 2018 ). However, again, the choice of indicators – and also potentially of different appraisal concepts for indicators used for the same quality aspects – will depend on the exact purpose of measurement.
3.3. Different purposes of quality measurement and users of quality information
It is useful to distinguish between two main purposes of quality measurement: The first purpose is to use quality measurement in quality assurance systems as a summative mec h anism for external accountability and verification. The second purpose is to use quality measurement as a formative mechanism for quality improvement. Depending on the purpose, quality measurement systems face different challenges with regard to indicators, data sources and the level of precision required.
Table 3.1 highlights the differences between quality assurance and quality improvement (Freeman, 2002 ; Gardner, Olney & Dickinson, 2018 ). Measurement for quality assurance and accountability is focused on identifying and overcoming problems with quality of care and assuring a sufficient level of quality across providers. Quality assurance is the focus of many external assessment strategies ( see also Chapter 8 ), and providers of insufficient quality may ultimately lose their licence and be prohibited from providing care. Assuring accountability is one of the main purposes of public reporting initiatives ( see Chapter 13 ), and measured quality of care may contribute to trust in healthcare services and allow patients to choose higher-quality providers.
The purpose of quality measurement: quality assurance versus quality improvement.
Quality measurement for quality assurance and accountability makes summative judgements about the quality of care provided. The idea is that “real” differences will be detected as a result of the measurement initiative. Therefore, a high level of precision is necessary and advanced statistical techniques may need to be employed to make sure that detected differences between providers are “real” and attributable to provider performance. Otherwise, measurement will encounter significant justified resistance from providers because its potential consequences, such as losing the licence or losing patients to other providers, would be unfair. Appraisal concepts of indicators for quality assurance will usually focus on assuring a minimum quality of care and identifying poor-quality providers. However, if the purpose is to incentivize high quality of care through pay for quality initiatives, the appraisal concept will likely focus on identifying providers delivering excellent quality of care.
By contrast, measurement for quality improvement is change oriented and quality information is used at the local level to promote continuous efforts of providers to improve their performance. Indicators have to be actionable and hence are often more process oriented. When used for quality improvement, quality measurement does not necessarily need to be perfect because it is only informative. Other sources of data and local information are considered as well in order to provide context for measured quality of care. The results of quality measurement are only used to start discussions about quality differences and to motivate change in provider behaviour, for example, in audit and feedback initiatives ( see Chapter 10 ). Freeman ( 2002 ) sums up the described differences between quality improvement and quality assurance as follows: “Quality improvement models use indicators to develop discussion further, assurance models use them to foreclose it.”
Different stakeholders in healthcare systems pursue different objectives and as a result they have different information needs (Smith et al., 2009 ; EC, 2016 ). For example, governments and regulators are usually focused on quality assurance and accountability. They use related information mostly to assure that the quality of care provided to patients is of a sufficient level to avoid harm – although they are clearly also interested in assuring a certain level of effectiveness. By contrast, providers and professionals are more interested in using quality information to enable quality improvement by identifying areas where they deviate from scientific standards or benchmarks, which point to possibilities for improvement ( see Chapter 10 ). Finally, patients and citizens may demand quality information in order to be assured that adequate health services will be available in case of need and to be able to choose providers of good-quality care ( see Chapter 13 ). The stakeholders and their purposes of quality measurement have, of course, an important influence on the selection of indicators and data needs ( see below).
While the distinction between quality assurance and quality improvement is useful, the difference is not always clear-cut. First, from a societal perspective, quality assurance aims at stamping out poor-quality care and thus contributes to improving average quality of care. Secondly, proponents of several of the strategies that are included under quality assurance in Table 3.1 , such as external assessment ( see also Chapter 8 ) or public reporting ( see also Chapter 13 ), in fact claim that these strategies do contribute to improving quality of care and assuring public trust in healthcare services. In fact, as pointed out in the relevant chapters, the rationale of external assessment and public reporting is that these strategies will lead to changes within organizations that will ultimately contribute to improving quality of care. Clearly, there also need to be incentives and/or motivations for change, i.e. while internal quality improvement processes often rely on professionalism, external accountability mechanisms seek to motivate through external incentives and disincentives – but this is beyond the scope of this chapter.
3.4. Types of quality indicators
There are many options for classifying different types of quality indicators (Mainz, 2003 ). One option is to distinguish between rate-based indicators and simple count-based indicators, usually used for rare “sentinel” events. Rate-based indicators are the more common form of indicators. They are expressed as proportions or rates with clearly defined numerators and denominators, for example, the proportion of hip fracture patients who receive antibiotic prophylaxis before surgery. Count-based indicators are often used for operationalizing the safety dimension of quality and they identify individual events that are intrinsically undesirable. Examples include “never events”, such as a foreign body left in during surgery or surgery on the wrong side of the body. If the measurement purpose is quality improvement, each individual event would trigger further analysis and investigation to avoid similar problems in the future.
Another option is to distinguish between generic and disease-specific indicators. Generic indicators measure aspects of care that are relevant to all patients. One example of a generic indicator is the proportion of patients who waited more than six hours in the emergency department. Disease-specific indicators are relevant only for patients with a particular diagnosis, such as the proportion of patients with lung cancer who are alive 30 days after surgery.
Yet other options relate to the different lenses of the framework presented in Chapter 2 . Indicators can be classified depending on the dimension of quality that they assess, i.e. effectiveness, patient safety and/or patient-centredness (the first lens); and with regard to the assessed function of healthcare, i.e. prevention, acute, chronic and/or palliative care (the second lens). Furthermore, it is possible to distinguish between patient-based indicators and event-based indicators. Patient-based indicators are indicators that are developed based on data that are linked across settings, allowing the identification of the pathway of care provided to individual patients. Event-based indicators are related to a specific event, for example, a hospital admission.
However, the most frequently used framework for distinguishing between different types of quality indicators is Donabedian’s classification of structure, process and outcome indicators (Donabedian, 1980 ). Donabedian’s triad builds the fourth lens of the framework presented in Chapter 2 . The idea is that the structures where health care is provided have an effect on the processes of care, which in turn will influence patient health outcomes. Table 3.2 provides some examples of structure, process and outcome indicators related to the different dimensions of quality.
Examples of structure, process and outcome quality indicators for different dimensions of quality.
In general, structural quality indicators are used to assess the setting of care, such as the adequacy of facilities and equipment, staffing ratios, qualifications of medical staff and administrative structures. Structural indicators related to effectiveness include the availability of staff with an appropriate skill mix, while the availability of safe medicines and the volume of surgeries performed are considered to be more related to patient safety. Structural indicators for patient-centredness can include the organizational implementation of a patients’ rights charter or the availability of patient information. Although institutional structures are certainly important for providing high-quality care, it is often difficult to establish a clear link between structures and clinical processes or outcomes, which reduces, to a certain extent, the relevance of structural measures.
Process indicators are used to assess whether actions indicating high-quality care are undertaken during service provision. Ideally, process indicators are built on reliable scientific evidence that compliance with these indicators is related to better outcomes of care. Sometimes process indicators are developed on the basis of clinical guidelines ( see also Chapter 9 ) or some other golden standard. For example, a process indicator of effective care for AMI patients may assess if patients are given aspirin on arrival. A process indicator of safety in surgery may assess if a safety checklist is used during surgery, and process indicators for patient-centredness may analyse patient-reported experience measures (PREMs). Process measures account for the majority of most quality measurement frameworks (Cheng et al., 2014 ; Fujita, Moles & Chen, 2018 ; NQF, 2019a ).
Finally, outcome indicators provide information about whether healthcare services help people stay alive and healthy. Outcome indicators are usually concrete and highly relevant to patients. For example, outcome indicators of effective ambulatory care include hospitalization rates for preventable conditions. Indicators of effective inpatient care for patients with acute myocardial infarction often include mortality rates within 30 days after admission, preferably calculated as a patient-based indicator (i.e. capturing deaths in any setting outside the hospital) and not as an event-based indicator (i.e. capturing death only within the hospital). Outcome indicators of patient safety may include complications of treatment, such as hospital acquired infections or foreign bodies left in during surgery. Outcome indicators of patient-centredness may assess patient satisfaction or patients’ willingness to recommend the hospital. Outcome indicators are increasingly used in quality measurement programmes, in particular in the USA, because they are of greater interest to patients and payers (Baker & Chassin, 2017 ).
3.5. Advantages and disadvantages of different types of indicators
Different types of indicators have their various strengths and weaknesses:
- Generic indicators have the advantage that they assess aspects of healthcare quality that are relevant to all patients. Therefore, generic indicators are potentially meaningful for a greater audience of patients, payers and policy-makers.
- Disease-specific indicators are better able to capture different aspects of healthcare quality that are relevant for improving patient care. In fact, most aspects of healthcare quality are disease-specific because effectiveness, safety and patient-centredness mean different things for different groups of diseases. For example, prescribing aspirin at discharge is an indicator of providing effective care for patients after acute myocardial infarction. However, if older patients are prescribed aspirin for extended periods of time without receiving gastro-protective medicines, this is an indicator of safety problems in primary care (NHS BSA, 2019 ).
Likewise, structure, process and outcome indicators each have their comparative strengths and weaknesses. These are summarized in Table 3.3 . The strength of structural measures is that they are easily available, reportable and verifiable because structures are stable and easy to observe. However, the main weakness is that the link between structures and clinical processes or outcomes is often indirect and dependent on the actions of healthcare providers.
Strengths and weaknesses of different types of indicators.
Process indicators are also measured relatively easily, and interpretation is often straightforward because there is often no need for risk-adjustment. In addition, poor performance on process indicators can be directly attributed to the actions of providers, thus giving clear indication for improvement, for example, by better adherence to clinical guidelines (Rubin, Pronovost & Diette, 2001 ). However, healthcare is complex and process indicators usually focus only on very specific procedures for a specific group of patients. Therefore, hundreds of indicators are needed to enable a comprehensive analysis of the quality of care provided by a professional or an institution. Relying only on a small set of process indicators carries the risk of distorting service provision towards a focus on measured areas of care while disregarding other (potentially more) important tasks that are harder to monitor.
Outcome indicators place the focus of quality assessments on the actual goals of service provision. Outcome indicators are often more meaningful to patients and policy-makers. The use of outcome indicators may also encourage innovations in service provision if these lead to better outcomes than following established processes of care. However, attributing health outcomes to the services provided by individual organizations or professionals is often difficult because outcomes are influenced by many factors outside the control of a provider (Lilford et al., 2004 ). In addition, outcomes may require a long time before they manifest themselves, which makes outcome measures more difficult to use for quality measurement (Donabedian, 1980 ). Furthermore, poor performance on outcome indicators does not necessarily provide direct indication for action as the outcomes may be related to a range of actions of different individuals who worked in a particular setting at a prior point in time.
3.6. Aggregating information in composite indicators
Given the complexity of healthcare provision and the wide range of relevant quality aspects, many quality measurement systems produce a large number of quality indicators. However, the availability of numerous different indicators may make it difficult for patients to select the best providers for their needs and for policy-makers to know whether overall quality of healthcare provision is improving. In addition, purchasers may struggle with identifying good-quality providers if they do not have a metric for aggregating conflicting results from different indicators. As a result, some users of quality information might base their decisions on only a few selected indicators that they understand, although these may not be the most important ones, and the information provided by many other relevant indicators will be lost (Goddard & Jacobs, 2009 ).
In response to these problems, many quality measurement initiatives have developed methods for combining different indicators into composite indicators or composite scores (Shwartz, Restuccia & Rosen, 2015 ). The use of composite indicators allows the aggregation of different aspects of quality into one measure to give a clearer picture of the overall quality of healthcare providers. The advantage is that the indicator summarizes information from a potentially wide range of individual indicators, thus providing a comprehensive assessment of quality. Composite indicators can serve many purposes: patients can select providers based on composite scores; hospital managers can use composite indicators to benchmark their hospitals against others, policy-makers can use composite indicators to assess progress over time, and researchers can use composite indicators for further analyses, for example, to identify factors associated with good quality of care. Table 3.4 summarizes some of the advantages and disadvantages of composite indicators.
Advantages and disadvantages of composite indicators.
The main disadvantages of composite indicators include that there are different (valid) options for aggregating individual indicators into composite indicators and that the methodological choices made during indicator construction will influence the measured performance. In addition, composite indicators may lead to simplistic conclusions and disguise serious failings in some dimensions. Furthermore, because of the influence of methodological choices on results, the selection of constituting indicators and weights could become the subject of political dispute. Finally, composite indicators do not allow the identification of specific problem areas and thus they need to be used in conjunction with individual quality indicators in order to enable quality improvement.
There are at least three important methodological choices that have to be made to construct a composite indicator. First, individual indicators have to be chosen to be combined in the composite indicator. Of course, the selection of indicators and the quality of chosen indicators will be decisive for the reliability of the overall composite indicator. Secondly, individual indicators have to be transformed into a common scale to enable aggregation. There are many methods available for this rescaling of the results, including ranking, normalizing (for example, using z-scores), calculating the proportion of the range of scores, and grouping scores into categories (for example, 5 stars) (Shwartz, Restuccia & Rosen, 2015 ). All of these methods have their comparative advantages and disadvantages and there is no consensus about which one should be used for the construction of composite indicators.
Thirdly, weights have to be attached to the individual indicators, which signal the relative importance of the different components of the composite indicator. Potentially, the ranking of providers can change dramatically depending on the weights given to individual indicators (Goddard & Jacobs, 2009 ). Again, several options exist. The most straightforward way is to use equal weights for every indicator but this is unlikely to reflect the relative importance of individual measures. Another option is to base the weights on expert judgement or preferences of the target audience. Further options include opportunity-based weighting, also called denominator-based weights because more weight is given to indicators for more prevalent conditions (for example, higher weights for diabetes-related indicators than for acromegaly-related indicators), and numerator-based weights which give more weight to indicators covering a larger number of events (for example, higher weight on medication interaction than on wrong-side surgery). Finally, yet another option is to use an all-or-none approach at the patient level, where a score of one is given only if all requirements for an individual patient have been met (for example, all five recommended pre-operative processes were performed).
Again, there is no clear guidance on how best to construct a composite indicator. However, what is important is that indicator construction is transparent and that methodological choices and rationales are clearly explained to facilitate understanding. Furthermore, different choices will provide different incentives for improvement and these need to be considered during composite construction.
3.7. Selection of indicators
A wide range of existing indicators is available that can form the basis for the development of new quality measurement initiatives. For example, the National Quality Forum (NQF) in the USA provides an online database with more than a thousand quality indicators that can be searched by type of indicator (structure, process, outcome), by clinical area (for example, dental, cancer or eye care), by target of measurement (for example, provider, payer, population), and by endorsement status (i.e. whether they meet the NQF’s measure evaluation criteria) (NQF, 2019a ). The OECD Health Care Quality Indicator Project provides a list of 55 quality indicators for cross-country analyses of the quality of primary care, acute care and mental care, as well as patient safety and patient experiences (OECD HCQI, 2016 ). The Australian Commission on Safety and Quality in Health Care has developed a broad set of indicators for hospitals, primary care, patient safety and patient experience, among others (ACSQHC, 2019 ).
The English Quality and Outcomes Framework (QOF) includes 77 indicators for evaluating the quality of primary care (NHS Employers, 2018 ), and these indicators have inspired several other countries to develop their own quality indicators for primary care. The NHS also publishes indicators for the assessment of medication safety (NHS BSA, 2019 ). In addition, several recent reviews have summarized available quality indicators for different areas of care, for example, palliative care (Pfaff & Markaki, 2017 ), mental health (Parameswaran, Spaeth-Rublee & Alan Pincus, 2015 ), primary care for patients with serious mental illnesses (Kronenberg et al., 2017 ), cardiovascular care (Campbell et al., 2008 ), and for responsible use of medicines (Fujita, Moles & Chen, 2018 ). Different chapters in this book will refer to indicators as part of specific quality strategies such as public reporting ( see Chapter 13 ).
In fact, there is a plethora of indicators that can potentially be used for measurement for the various purposes described previously ( see section above: Different purposes of quality measurement and users of quality information). However, because data collection and analysis may consume considerable resources, and because quality measurement may have unintended consequences, initiatives have to carefully select (or newly develop) indicators based on the identified quality problem, the interested stakeholders and the purpose of measurement (Evans et al., 2009 ).
Quality measurement that aims to monitor and/or address problems related to specific diseases, for example, cardiovascular or gastrointestinal diseases, or particular groups of patients, for example, geriatric patients or paediatric patients, will likely require disease-specific indicators. By contrast, quality measurement aiming to address problems related to the organization of care (for example, waiting times in emergency departments), to specific providers (for example, falls during inpatient stays), or professionals (for example, insufficiently qualified personnel) will likely require generic indicators. Quality problems related to the effectiveness of care are likely to require rate-based disease-specific indicators, while safety problems are more likely to be addressed through (often generic) sentinel event indicators. Problems with regard to patient-centredness will likely require indicators based on patient surveys and expressed as rates.
The interested stakeholders and the purpose of measurement should determine the desired level of detail and the focus of measurement on structures, processes or outcomes. This is illustrated in Table 3.5 , which summarizes the information needs of different stakeholders in relation to their different purposes. For example, governments responsible for assuring overall quality and accountability of healthcare service provision will require relatively few aggregated composite indicators, mostly of health outcomes, to monitor overall system level performance and to assure value for money. By contrast, provider organizations and professionals, which are mostly interested in quality improvement, are likely to demand a high number of disease-specific process indicators, which allows identification of areas for quality improvement.
Information needs of health system stakeholders with regard to quality of care.
Another issue that needs to be considered when choosing quality indicators is the question of finding the right balance between coverage and practicality. Relying on only a few indicators causes some aspects of care quality to be neglected and potentially to distract attention away from non-measured areas. It may also be necessary to have more than one indicator for one quality aspect, for example, mortality, readmissions and a PREM. However, maintaining too many indicators will be expensive and impractical to use. Finally, the quality of quality indicators should be a determining factor in selecting indicators for measurement.
3.8. Quality of quality indicators
There are numerous guidelines and criteria available for evaluating the quality of quality indicators. In 2006 the OECD Health Care Quality Indicators Project published a list of criteria for the selection of quality indicators (Kelley & Hurst, 2006 ). A relatively widely used tool for the evaluation of quality indicators has been developed at the University of Amsterdam, the Appraisal of Indicators through Research and Evaluation (AIRE) instrument (de Koning, Burgers & Klazinga, 2007 ). The NQF in the USA has published its measure evaluation criteria, which form the basis for evaluations of the eligibility of quality indicators for endorsement (NQF, 2019b ). In Germany yet another tool for the assessment of quality indicators – the QUALIFY instrument – was developed by the Federal Office for Quality Assurance (BQS) in 2007, and the Institute for Quality Assurance and Transparency in Health Care (IQTIG) defined a similar set of criteria in 2018 (IQTIG, 2018 ).
In general, the criteria defined by the different tools are quite similar but each tool adds certain aspects to the list. Box 3.1 summarizes the criteria defined by the various tools grouped along the dimensions of relevance, scientific soundness, feasibility and meaningfulness. The relevance of an indicator can be determined based on its effect on health or health expenditures, the importance that it has for the relevant stakeholders, the potential for improvement (for example, as determined by available evidence about practice variation), and the clarity of the purpose and the healthcare context for which the indicator was developed. The latter point is important because many of the following criteria are dependent on the specific purpose.
Criteria for indicators.
For example, the desired level for the criteria of validity, sensitivity and specificity will differ depending on whether the purpose is external quality assurance or internal quality improvement. Similarly, if the purpose is to assure a minimum level of quality across all providers, the appraisal concept has to focus on minimum acceptable requirements, while it will have to distinguish between good and very good performers if the aim is to reward high-quality providers through a pay for quality approach ( see Chapter 14 ).
Important aspects that need to be considered with regard to feasibility of measurement include whether previous experience exists with the use of the measure, whether the necessary information is available or can be collected in the required timeframe, whether the costs of measurement are acceptable, and whether the data will allow meaningful analyses for relevant subgroups of the population (for example, by socioeconomic status). Furthermore, the meaningfulness of the indicator is an important criterion, i.e. whether the indicator allows useful comparisons, whether the results are user-friendly for the target audience, and whether the distinction between high and low quality is meaningful for the target audience.
3.9. Data sources for measuring quality
Many different kinds of data are available that can potentially be used for quality measurement. The most often used data sources are administrative data, medical records of providers and data stored in different – often disease-specific – registers, such as cancer registers. In addition, surveys of patients or healthcare personnel can be useful to gain additional insights into particular dimensions of quality. Finally, other approaches, such as direct observation of a physician’s activities by a qualified colleague, are useful under specific conditions (for example, in a research context) but usually not possible for continuous measurement of quality.
There are many challenges with regard to the quality of the available data. These challenges can be categorized into four key aspects: (1) completeness, (2) comprehensiveness, (3) validity and (4) timeliness. Completeness means that the data properly include all patients with no missing cases. Comprehensiveness refers to whether the data contain all relevant variables needed for analysis, such as diagnosis codes, results of laboratory tests or procedures performed. Validity means that the data accurately reflect reality and are free of bias and errors. Finally, timeliness means that the data are available for use without considerable delay.
Data sources differ in their attributes and have different strengths and weaknesses, which are presented below and summarized in Table 3.6 . The availability of data for research and quality measurement purposes differs substantially between countries. Some countries have more restrictive data privacy protection legislation in place, and also the possibility of linking different databases using unique personal identifiers is not available in all countries (Oderkirk, 2013 ; Mainz, Hess & Johnsen, 2019 ). Healthcare providers may also use patient data only for internal quality improvement purposes and prohibit transfer of data to external bodies. Nevertheless, with the increasing diffusion of IT technology in the form of electronic health records, administrative databases and clinical registries, opportunities of data linkage are increasing, potentially creating new and better options for quality measurement.
Strengths and weaknesses of different data sources.
3.9.1. Administrative data
Administrative data are not primarily generated for quality or research purposes but by definition for administrative and management purposes (for example, billing data, routine documentation) and have the advantage of being readily available and easily accessible in electronic form. Healthcare providers, in particular hospitals, are usually mandated to maintain administrative records, which are used in many countries for quality measurement purposes. In addition, governments usually have registers of births and deaths that are potentially relevant for quality measurement but which are often not used by existing measurement systems.
Administrative discharge data from hospitals usually include a patient identifier, demographic information, primary and secondary diagnoses coded using the International Classification of Diseases (ICD), coded information about medical and surgical procedures, dates of services provided, provider identifiers and many other bits of information (Iezzoni, 2009 ).
However, more detailed clinical information on severity of disease (for example, available from lab test results) or information about functional impairment or quality of life are not available in administrative data. The strength of administrative data is that they are comprehensive and complete with few problems of missing data. The most important problem of administrative data is that they are generated by healthcare providers, usually for payment purposes. This means that coding may be influenced by the incentives of the payment system, and – once used for purposes of quality measurement – also by incentives attached to the measured quality of care.
3.9.2. Medical record data
Medical records contain the most in-depth clinical information and document the patient’s condition or problem, tests and treatments received and follow-up care. The completeness of medical record data varies greatly between and within countries and healthcare providers. Especially in primary care where the GP is familiar with the patient, proper documentation is often lacking. Also, if the patient changes provider during the treatment process and each provider keeps their own medical records, the different records would need to be combined to get a complete picture of the process (Steinwachs & Hughes, 2008 ).
Abstracting information from medical records can be expensive and time-consuming since medical records are rarely standardized. Another important aspect is to make sure that the information from medical records is gathered in a systematic way to avoid information bias. This can be done by defining clinical variables explicitly, writing detailed abstraction guidelines and training staff to maintain data quality. Medical record review is used mostly in internal quality improvement initiatives and research studies.
With the growth of electronic medical and electronic health records, the use of this data for more systematic quality measurement will likely increase in the future. The potential benefits of using electronic records are considerable as this may allow real-time routine analysis of the most detailed clinical information available, including information from imaging tests, prescriptions and pathology systems (Kannan et al., 2017 ). However, it will be necessary to address persisting challenges with regard to accuracy, completeness and comparability of the data collected in electronic records to enable reliable measurement of quality of care on the basis of this data (Chan et al., 2010 ).
3.9.3. Disease-specific registries
There are many disease-specific registries containing data that can be used for healthcare quality measurement purposes. Cancer registries exist in most developed countries and, while their main purpose is to register cancer cases and provide information on cancer incidence in their catchment area, the data can also be used for monitoring and evaluation of screening programmes and estimating cancer survival by follow-up of cancer patients (Bray & Parkin, 2009 ). In Scandinavian countries significant efforts have gone into standardizing cancer registries to enable cross-country comparability. Nevertheless, numerous differences persist with regard to registration routines and classification systems, which are important when comparing time trends in the Nordic countries (Pukkala et al., 2018 ).
In some countries there is a large number of clinical registries that are used for quality measurement. For example, in Sweden there are over a hundred clinical quality registries, which work on a voluntary basis as all patients must be informed and have the right to opt-out. These registries are mainly for specific diseases and they include disease-specific data, such as severity of disease at diagnosis, diagnostics and treatment, laboratory tests, patient-reported outcome measures, and other relevant factors such as body mass index, smoking status or medication. Most of the clinical registries focus on specialized care and are based on reporting from hospitals or specialized day care centres (Emilsson et al., 2015 ).
With increasing diffusion of electronic health records, it is possible to generate and feed disease-specific population registries based on electronic abstraction (Kannan et al., 2017 ). Potentially, this may significantly reduce the costs of data collection for registries. Furthermore, linking of data from different registries with other administrative data sources can increasingly be used to generate datasets that enable more profound analyses.
3.9.4. Survey data
Survey data are another widely used source of quality information. Surveys are the only option for gaining information about patient experiences with healthcare services and thus are an important source of information about patient-centredness of care. Substantial progress has been made over recent years to improve standardization of both patient-reported experience measures (PREMs) and patient-reported outcome measures (PROMs) in order to facilitate international comparability (Fujisawa & Klazinga, 2017 ).
Surveys of patient experiences capture the patients’ views on health service delivery (for example, communication with nurses and doctors, staff responsiveness, discharge and care coordination). Most OECD countries have developed at least one national survey measuring PREMs over the past decade or so (Fujisawa & Klazinga, 2017 ), and efforts are under way to further increase cooperation and collaboration to facilitate comparability (OECD, 2017 ).
Surveys of patient-reported outcomes capture the patient’s perspective on their health status (for example, symptoms, functioning, mental health). PROMs surveys can use generic tools (for example, the SF-36 or EQ-5D) or disease-specific tools, which are usually more sensitive to change (Fitzpatrick, 2009 ). The NHS in the United Kingdom requires all providers to report PROMs for two elective procedures: hip replacement and knee replacement. Both generic (EQ-5D and EQ VAS) and disease-specific (Oxford Hip Score, Oxford Knee Score and Aberdeen Varicose Vein Questionnaire) instruments are used (NHS Digital, 2019b ).
Finally, several countries also use surveys of patient satisfaction in order to monitor provider performance. However, satisfaction is difficult to compare internationally because it is influenced by patients’ expectations about how they will be treated, which vary widely across countries and also within countries (Busse, 2012 ).
3.9.5. Direct observation
Direct observation is sometimes used for research purposes or as part of peer-review processes. Direct observation allows the study of clinical processes, such as the adherence to clinical guidelines and the availability of basic structures. Observation is normally considered to be too resource-intensive for continuous quality measurement. However, site visits and peer-reviews are often added to routine monitoring of secondary (administrative) data to investigate providers with unexplained variation in quality and to better understand the context where these data are produced.
3.10. Attribution and risk-adjustment
Two further conceptual and methodological considerations are essential when embarking on quality measurement or making use of quality data, in particular with regard to outcome indicators. Both are related to the question of responsibility for differences in measured quality of care or, in other words, related to the question of attributing causality to responsible agents (Terris & Aron, 2009 ). Ideally, quality measurement is based on indicators that have been purposefully developed to reflect the quality of care provided by individuals, teams, provider organizations (for example, hospitals) or other units of analysis (for example, networks, regions, countries) ( see also above, Quality of quality indicators). However, many existing quality indicators do not reflect only the quality of care provided by the target of measurement but also a host of factors that are outside the direct control of an individual provider or provider organization.
For example, surgeon-specific mortality data for patients undergoing coronary artery bypass graft (CABG) have been publicly reported in England and several states of the USA for many years (Radford et al., 2015 ; Romano et al., 2011 ). Yet debate continues whether results actually reflect the individual surgeon’s quality of care or rather the quality of the wider hospital team (for example, including anaesthesia, intensive care unit quality) or the organization and management of the hospital (for example, the organization of resuscitation teams within hospitals) (Westaby et al., 2015 ). Nevertheless, with data released at the level of the surgeon, responsibility is publicly attributed to the individual and not to the organization.
Other examples where attributing causality and responsibility is difficult include outcome indicators defined using time periods (for example, 30-day mortality after hospitalization for ischemic stroke) because patients may be transferred between different providers and because measured quality will depend on care received after discharge. Similarly, attribution can be problematic for patients with chronic conditions, for example, attributing causality for hospitalizations of patients with heart failure – a quality indicator in the USA – is difficult because these patients may see numerous providers, such as one (or more) primary care physician(s) and specialists, for example, nephrologists and/or cardiologists.
What these examples illustrate is that attribution of quality differences to providers is difficult. However, it is important to accurately attribute causality because it is unfair to hold individuals or organizations accountable for factors outside their control. In addition, if responsibility is attributed incorrectly, quality improvement measures will be in vain, as they will miss the appropriate target. Therefore, when developing quality indicators, it is important that a causal pathway can be established between the agents under assessment and the outcome proposed as a quality measure. Furthermore, possible confounders, such as the influence of other providers or higher levels of the healthcare system on the outcome of interest, should be carefully explored in collaboration with relevant stakeholders (Terris & Aron, 2009 ).
Of course, many important confounders outside the control of providers have not yet been mentioned as the most important confounders are patient-level clinical factors and patient preferences. Prevalence of these factors may differ across patient populations and influence the outcomes of care. For example, severely ill patients or patients with multiple coexisting conditions are at risk of having worse outcomes than healthy individuals despite receiving high-quality care. Therefore, providers treating sicker patients are at risk of performing poorly on measured quality of care, in particular when measured through outcome indicators.
Risk-adjustment (sometimes called case-mix adjustment) aims to control for these differences (risk-factors) that would otherwise lead to biased results. Almost all outcome indicators require risk-adjustment to adjust for patient-level risk factors that are outside the control of providers. In addition, healthcare processes may be influenced by patients’ attitudes and perceptions, which should be taken into account for risk-adjustment of process indicators if relevant. Ideally, risk-adjustment assures that measured differences in the quality of care are not biased by differences in the underlying patient populations treated by different providers or in different regions.
An overview of potential patient (risk-) factors that may influence outcomes of care is presented in Table 3.7 . Demographic characteristics (for example, age), clinical (for example, co-morbidities) and socioeconomic factors, health-related behaviours (for example, alcohol use, nutrition) and attitudes may potentially have an effect on outcomes of care. By controlling for these factors, risk-adjustment methods will produce estimates that are better comparable across individuals, provider organizations or other units of analysis.
Potential patient risk-factors.
The field of risk-adjustment is developing rapidly and increasingly sophisticated methods are available for ensuring fair comparisons across providers, especially for conditions involving surgery, risk of death and post-operative complications (Iezzoni, 2009 ). Presentation of specific risk-adjustment methods is beyond the scope of this chapter but some general methods include direct and indirect standardization, multiple regression analysis and other statistical techniques. The selection of potential confounding factors needs to be done carefully, taking into account the ultimate purpose and use of the quality indicator that needs adjustment.
In fact, the choice of risk-adjustment factors is not a purely technical exercise but relies on assumptions that are often not clearly spelled out. For example, in several countries the hospital readmission rate is used as a quality indicator in pay for quality programmes (Kristensen, Bech & Quentin, 2015 ). If it is believed that age influences readmission rates in a way hospitals cannot affect, age should be included in the risk-adjustment formula. However, if it is thought that hospitals can influence elderly patients’ readmission rates by special discharge programmes for the elderly, age may not be considered a “risk” but rather an indicator for the hospitals to use for identifying patients with special needs. The same arguments apply also for socioeconomic status. On the one hand, there are good reasons to adjust for socioeconomic variables because patients living in poorer neighbourhoods tend to have higher readmission rates. On the other hand, including socioeconomic variables in a risk-adjustment formula would implicitly mean that it was acceptable for hospitals located in poorer areas to have more readmissions.
The assumptions and methodological choices made when selecting variables for risk-adjustment may have a powerful effect on risk-adjusted measured quality of care. Some critics (for example, Lilford et al., 2004 ) have argued that comparative outcome data should not be used externally to make judgements about quality of hospital care. More recent criticism of risk-adjustment methods has suggested that risk-adjustment methods of current quality measurement systems could be evaluated by assigning ranks similar to those used to rate the quality of evidence (Braithwaite, 2018 ). Accordingly, A-level risk-adjustment would adjust for all known causes of negative consequences that are beyond the control of clinicians yet influence outcomes. C-level risk-adjustment would fail to control for several important factors that cause negative consequences, while B-level risk-adjustment would be somewhere in between.
3.11. Conclusion
This chapter has introduced some basic concepts and methods for the measurement of healthcare quality and presented a number of related challenges. Many different stakeholders have varying needs for information on healthcare quality and the development of quality measurement systems should always take into account the purpose of measurement and the needs of different stakeholders. Quality measurement is important for quality assurance and accountability to make sure that providers are delivering good-quality care but they are also vital for quality improvement programmes to ensure that these interventions lead to increases in care quality.
The development and use of quality measures should always be fit-for-purpose. For example, outcome-based quality indicators, such as those used by the OECD, are useful for international comparisons or national agenda-setting but providers such as hospitals or health centres may need more specific indicators related to processes of care in order to enable quality improvement. The Donabedian framework of structure, process and outcome indicators provides a comprehensive, easily understandable model for classifying different types of indicator, and it has guided indicator development of most existing quality measurement systems.
Quality indicators should be of high quality and should be carefully chosen and implemented in cooperation with providers and clinicians. The increasing availability of clinical data in the form of electronic health records is multiplying possibilities for quality measurement on the basis of more detailed indicators. In addition, risk-adjustment is important to avoid high-quality providers being incorrectly and unfairly identified as providing poor quality of care – and vice versa, to avoid that poor providers appear to be providing good quality of care. Again, the increasing availability of data from electronic medical records may expand the options for better risk-adjustment.
However, most quality measurement initiatives will continue to focus – for reasons of practicality and data availability – only on a limited set of quality indicators. This means that one of the fundamental risks of quality measurement will continue to be important: quality measurement will always direct attention to those areas that are covered by quality indicators, potentially at the expense of other important aspects of quality that are more difficult to assess through quality measurement.
Nevertheless, without quality information policy-makers lack the knowledge base to steer health systems, patients can only rely on personal experiences or those of friends for choosing healthcare providers, and healthcare providers have no way of knowing whether their quality improvement programmes have worked as expected.
Quality information is a tool and it can do serious damage if used inappropriately. Seven basic principles of using quality indicators are summarized in Box 3.2 . It is critical to be aware of the limitations of quality measurement and to be cautious of using quality information for quality strategies that provide powerful incentives to providers, such as public reporting ( see Chapter 13 ) or P4Q schemes ( see Chapter 14 ), as these may lead to potential unintended consequences such as gaming or patient selection.
Seven principles to take into account when using quality indicators.
- ACSQHC. Indicators of Safety and Quality. Australian Commission on Safety and Quality in Health Care (ACSQHC). 2019. https://www .safetyandquality .gov.au/our-work /indicators/#Patientreported , accessed 21 March 2019.
- Baker DW, Chassin MR. Holding Providers Accountable for Health Care Outcomes. Annals of Internal Medicine . 2017; 167 (6):418–23. [ PubMed : 28806793 ]
- Braithwaite RS. Risk Adjustment for Quality Measures Is Neither Binary nor Mandatory. Journal of the American Medical Association . 2018; 319 (20):2077–8. [ PubMed : 29710277 ]
- Bray F, Parkin DM. Evaluation of data quality in the cancer registry: Principles and methods. Part I: Comparability, validity and timeliness. European Journal of Cancer . 2009; 45 (5):747–55. [ PubMed : 19117750 ]
- Busse R. Being responsive to citizens’ expectations: the role of health services in responsiveness and satisfaction. In: McKee M, Figueras J (eds.), editors. Health Systems: Health, wealth and societal well-being. Maidenhead: Open University Press/McGraw-Hill; 2012.
- Calhoun C. Oxford dictionary of social sciences. New York: Oxford University Press; 2002.
- Campbell SM, et al. Quality indicators for the prevention and management of cardiovascular disease in primary care in nine European countries. European Journal of Cardiovascular Prevention & Rehabilitation . 2008; 15 (5):509–15. [ PubMed : 18695594 ]
- Carinci F, et al. Towards actionable international comparisons of health system performance: expert revision of the OECD framework and quality indicators. International Journal for Quality in Health Care . 2015; 27 (2):137–46. [ PubMed : 25758443 ]
- Chan KS, et al. Electronic health records and the reliability and validity of quality measures: a review of the literature. Medical Care Research and Review . 2010; 67 (5):503–27. [ PubMed : 20150441 ]
- Cheng EM, et al. Quality measurement: here to stay. Neurology Clinical Practice . 2014; 4 (5):441–6. [ PMC free article : PMC4196461 ] [ PubMed : 25317378 ]
- Cylus J, Papanicolas I, Smith P. Health system efficiency: how to make measurement matter for policy and management. Copenhagen: WHO, on behalf of the European Observatory on Health Systems and Policies; 2016. [ PubMed : 28783269 ]
- Davies H. Measuring and reporting the quality of health care: issues and evidence from the international research literature. NHS Quality Improvement Scotland; 2005.
- Donabedian A. The Definition of Quality and Approaches to Its Assessment. Vol 1. Explorations in Quality Assessment and Monitoring. Ann Arbor, Michigan, USA: Health Administration Press; 1980.
- EC. So What? Strategies across Europe to assess quality of care. Report by the Expert Group on Health Systems Performance Assessment. European Commission (EC). Brussels: European Commission; 2016.
- Emilsson L, et al. Review of 103 Swedish Healthcare Quality Registries. Journal of Internal Medicine . 2015; 277 (1):94–136. [ PubMed : 25174800 ]
- Evans SM, et al. Prioritizing quality indicator development across the healthcare system: identifying what to measure. Internal Medic ine Journal . 2009; 39 (10):648–54. [ PubMed : 19371394 ]
- Fitzpatrick R. Patient-reported outcome measures and performance measurement. In: Smith P, et al. (eds.), editors. Performance Measurement for Health System Improvement: Experiences, Challenges and Prospects. Cambridge: Cambridge University Press; 2009.
- Forde I, Morgan D, Klazinga N. Resolving the challenges in the international comparison of health systems: the must do’s and the trade-offs. Health Policy . 2013; 112 (1–2):4–8. [ PubMed : 23434265 ]
- Freeman T. Using performance indicators to improve health care quality in the public sector: a review of the literature. Health Services Management Research . 2002; 15 :126–37. [ PubMed : 12028801 ]
- Fujisawa R, Klazinga N. Measuring patient experiences (PREMS): Progress made by the OECD and its member countries between 2006 and 2016. Paris: Organisation for Economic Co-operation and Development (OECD); 2017.
- Fujita K, Moles RJ, Chen TF. Quality indicators for responsible use of medicines: a systematic review. BMJ Open . 2018; 8 :e020437. [ PMC free article : PMC6082479 ] [ PubMed : 30012782 ]
- Gardner K, Olney S, Dickinson H. Getting smarter with data: understanding tensions in the use of data in assurance and improvement-oriented performance management systems to improve their implementation. Health Research Policy and Systems . 2018; 16 (125) [ PMC free article : PMC6303867 ] [ PubMed : 30577854 ]
- Goddard M, Jacobs R. Using composite indicators to measure performance in health care. In: Smith P, et al. (eds.), editors. Performance Measurement for Health System Improvement: Experiences, Challenges and Prospects. Cambridge: Cambridge University Press; 2009.
- Hurtado MP, Swift EK, Corrigan JM. Envisioning the National Health Care Quality Report. Washington, DC: National Academy Press; 2001. [ PubMed : 25057551 ]
- ICHOM. Standard Sets. International Consortium for Health Outcomes Measurement (ICHOM). 2019. https://www .ichom.org/standard-sets/ , accessed 8 February 2019.
- Iezzoni L. Risk adjustment for performance measurement. In: Smith P, et al. (eds.), editors. Performance Measurement for Health System Improvement: Experiences, Challenges and Prospects. Cambridge: Cambridge University Press; 2009.
- IQTIG. Methodische Grundlagen V1.1.s. Entwurf für das Stellungnahmeverfahren. Institut für Qualitätssicherung und Transparenz im Gesundheitswesen (IQTIG). 2018. Available at: https://iqtig .org/das-iqtig /grundlagen/methodische-grundlagen/ , accessed 18 March 2019.
- Kannan V, et al. Rapid Development of Specialty Population Registries and Quality Measures from Electronic Health Record Data. Methods of information in medicine . 2017; 56 (99):e74–e83. [ PMC free article : PMC5608102 ] [ PubMed : 28930362 ]
- Kelley E, Hurst J. Health Care Quality Indicators Project: Conceptual framework paper. Paris: Organization for Economic Co-operation and Development (OECD); 2006. Available at: https://www .oecd.org /els/health-systems/36262363.pdf , accessed on 22/03/2019.
- De Koning J, Burgers J, Klazinga N. Appraisal of indicators through research and evaluation (AIRE). 2007. Available at: https://www .zorginzicht .nl/kennisbank/PublishingImages /Paginas /AIRE-instrument/AIRE %20Instrument%202.0.pdf , accessed 21 March 2019.
- Kristensen SR, Bech M, Quentin W. A roadmap for comparing readmission policies with application to Denmark, England and the United States. Health Policy . 2015; 119 (3):264–73. [ PubMed : 25547401 ]
- Kronenberg C, et al. Identifying primary care quality indicators for people with serious mental illness: a systematic review. British Journal of General Practice . 2017; 67 (661):e519–e530. [ PMC free article : PMC5519123 ] [ PubMed : 28673958 ]
- Lawrence M, Olesen F. Indicators of Quality in Health Care. European Journal of General Practice . 1997; 3 (3):103–8.
- Lighter D. How (and why) do quality improvement professionals measure performance. International Journal of Pediatrics and Adolescent Medicine . 2015; 2 (1):7–11. [ PMC free article : PMC6372368 ] [ PubMed : 30805429 ]
- Lilford R, et al. Use and misuse of process and outcome data in managing performance of acute medical care: avoiding institutional stigma. Lancet . 2004; 363 (9424):1147–54. [ PubMed : 15064036 ]
- Lohr KN. Medicare: A Strategy for Quality Assurance. Washington (DC), US: National Academies Press; 1990.
- Lüngen M, Rath T. Analyse und Evaluierung des QUALIFY Instruments zur Bewertung von Qualitätsindikatoren anhand eines strukturierten qualitativen Interviews. Zeitschrift für Evidenz, Fortbildung und Qualität im Gesundheitswesen . 2011; 105 (1):38–43. [ PubMed : 21382603 ]
- Mainz J. Defining and classifying indicators for quality improvement. International J ournal for Quality in Health Care . 2003; 15 (6):523–30. [ PubMed : 14660535 ]
- Mainz J, Hess MH, Johnsen SP. Perspectives on Quality: the Danish unique personal identifier and the Danish Civil Registration System as a tool for research and quality improvement. International Journal for Quality in Health Care (efirst). 2019. https://doi .org/10.1093/intqhc/mzz008 . [ PubMed : 31220255 ]
- Marjoua Y, Bozic K. Brief history of quality movement in US healthcare. Current reviews in musculos keletal medicine . 2012; 5 (4):265–73. [ PMC free article : PMC3702754 ] [ PubMed : 22961204 ]
- NHS BSA. Medication Safety – Indicators Specification. NHS Business Services Authority (NHS BSA). 2019. Available at: https://www .nhsbsa.nhs .uk/sites/default/files /2019-02/Medication %20Safety%20-%20Indicators %20Specification.pdf , accessed 21 March 2019.
- NHS Digital. Indicator Methodology and Assurance Service. NHS Digital, Leeds. 2019a. Available at: https://digital .nhs.uk /services/indicator-methodology-and-assurance-service , accessed 18 March 2019.
- NHS Digital. Patient Reported Outcome Measures (PROMs). NHS Digital, Leeds. 2019b. Available at: https://digital .nhs.uk /data-and-information /data-tools-and-services /data-services /patient-reported-outcome-measures-proms , accessed 22 March 2019. [ PubMed : 30591362 ]
- NHS Employers. 2018/19 General Medical Services (GMS) contract Quality and Outcomes Framework (QOF). 2018. Available at: https://www .nhsemployers .org/-/media/Employers /Documents/Primary-care-contracts /QOF /2018-19/2018-19-QOF-guidance-for-stakeholders.pdf , accessed 21 March 2019.
- NQF. Quality Positioning System. National Quality Forum (NQF). 2019a. Available at: http://www .qualityforum .org/QPS/QPSTool.aspx , accessed 19 March 2019.
- NQF. Measure evaluation criteria. National Quality Forum (NQF). 2019b. Available at: http://www .qualityforum .org/measuring_performance /submitting_standards /measure_evaluation_criteria .aspx , accessed 19 March 2019.
- Oderkirk J. International comparisons of health system performance among OECD countries: opportunities and data privacy protection challenges. Health Policy . 2013; 112 (1–2):9–18. [ PubMed : 23870099 ]
- OECD. Handbook on Constructing Composite Indicators: Methodology and user guide. Organisation for Economic Co-operation and Development (OECD). 2008. Available at: https://www .oecd.org/sdd/42495745.pdf , accessed 22 March 2019.
- OECD. Improving Value in Health Care: Measuring Quality. Organisation for Economic Co-operation and Development. 2010. Available at: https://www .oecd-ilibrary .org/docserver/9789264094819-en .pdf?expires =1545066637&id =id&accname =ocid56023174a&checksum =1B31D6EB98B6160BF8A5265774A54D61 , accessed 17 December 2018.
- OECD. Strengthening the international comparison of health system performance through patient-reported indicators. Paris: Organisation for Economic Co-operation and Development; 2017. Recommendations to OECD Ministers of Health from the High Level Reflection Group on the future of health statistics.
- OECD. Patient-Reported Indicators Survey (PaRIS). Paris: Organisation for Economic Co-operation and Development; 2019. Available at: http://www .oecd.org/health/paris.htm , accessed 8 February 2019.
- OECD HCQI. Definitions for Health Care Quality Indicators 2016–2017. HCQI Data Collection. Organisation for Economic Co-operation and Development Health Care Quality Indicators Project. 2016. Available at: http://www .oecd.org/els /health-systems/Definitions-of-Health-Care-Quality-Indicators.pdf , accessed 21 March 2019.
- Papanicolas I, Smith P. WHO, on behalf of the European Observatory. Open University Press; Maidenhead: 2013. Health system performance comparison: an agenda for policy, information and research.
- Parameswaran SG, Spaeth-Rublee B, Alan Pincus H. Measuring the Quality of Mental Health Care: Consensus Perspectives from Selected Industrialized Countries. Administration and Policy in Mental Health . 2015; 42 :288–95. [ PubMed : 24951953 ]
- Pfaff K, Markaki A. Compassionate collaborative care: an integrative review of quality indicators in end-of-life care. BMC Palliative Care . 2017; 16 :65. [ PMC free article : PMC5709969 ] [ PubMed : 29191185 ]
- Porter M. What is value in health care. New England Journal of Medicine . 2010; 363 (26):2477–81. [ PubMed : 21142528 ]
- Pukkala E, et al. Nordic Cancer Registries – an overview of their procedures and data comparability. Acta Oncologica . 2018; 57 (4):440–55. [ PubMed : 29226751 ]
- Radford PD, et al. Publication of surgeon specific outcome data: a review of implementation, controversies and the potential impact on surgical training. International Journal of Surgery . 2015; 13 :211–16. [ PubMed : 25498494 ]
- Romano PS, et al. Impact of public reporting of coronary artery bypass graft surgery performance data on market share, mortality, and patient selection. Medical Care . 2011; 49 (12):1118–25. [ PubMed : 22002641 ]
- Rubin HR, Pronovost P, Diette G. The advantages and disadvantages of process-based measures of health care quality. Interna tional Journal for Quality in Health Care . 2001; 13 (6):469–74. [ PubMed : 11769749 ]
- Shwartz M, Restuccia JD, Rosen AK. Composite Measures of Health Care Provider Performance: A Description of Approaches. Milbank Quarterly . 2015; 93 (4):788–825. [ PMC free article : PMC4678940 ] [ PubMed : 26626986 ]
- Smith P, et al. Introduction. In: Smith P, et al. (eds.), editors. Performance Measurement for Health System Improvement: Experiences, Challenges and Prospects. Cambridge: Cambridge University Press; 2009.
- Steinwachs DM, Hughes RG. Patient Safety and Quality: An Evidence-Based Handbook for Nurses. Rockville (MD): Agency for Healthcare Research and Quality (US); 2008. Health Services Research: Scope and Significance. [ PubMed : 21328752 ]
- Terris DD, Aron DC. Attribution and causality in health-care performance measurement. In: Smith P, et al. (eds.), editors. Performance Measurement for Health System Improvement: Experiences, Challenges and Prospects. Cambridge: Cambridge University Press; 2009.
- Voeten SC, et al. Quality indicators for hip fracture care, a systematic review. Osteoporosis International . 2018; 29 (9):1963–85. [ PMC free article : PMC6105160 ] [ PubMed : 29774404 ]
- Westaby S, et al. Surgeon-specific mortality data disguise wider failings in delivery of safe surgical services. European Journal of Cardiothoracic Surgery . 2015; 47 (2):341–5. [ PubMed : 25354748 ]
- Cite this Page Quentin W, Partanen VM, Brownwood I, et al. Measuring healthcare quality. In: Busse R, Klazinga N, Panteli D, et al., editors. Improving healthcare quality in Europe: Characteristics, effectiveness and implementation of different strategies [Internet]. Copenhagen (Denmark): European Observatory on Health Systems and Policies; 2019. (Health Policy Series, No. 53.) 3.
- PDF version of this title (4.8M)
In this Page
- Introduction
- How can quality be measured? From a concept of quality to quality indicators
- Different purposes of quality measurement and users of quality information
- Types of quality indicators
- Advantages and disadvantages of different types of indicators
- Aggregating information in composite indicators
- Selection of indicators
- Quality of quality indicators
- Data sources for measuring quality
- Attribution and risk-adjustment
Other titles in this collection
- European Observatory Health Policy Series
Related information
- PMC PubMed Central citations
- PubMed Links to PubMed
Recent Activity
- Measuring healthcare quality - Improving healthcare quality in Europe Measuring healthcare quality - Improving healthcare quality in Europe
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers
- Open access
- Published: 22 August 2023
Quality communication can improve patient-centred health outcomes among older patients: a rapid review
- Samer H. Sharkiya 1
BMC Health Services Research volume 23 , Article number: 886 ( 2023 ) Cite this article
76k Accesses
44 Citations
19 Altmetric
Metrics details
Effective communication is a cornerstone of quality healthcare. Communication helps providers bond with patients, forming therapeutic relationships that benefit patient-centred outcomes. The information exchanged between the provider and patient can help in medical decision-making, such as better self-management. This rapid review investigated the effects of quality and effective communication on patient-centred outcomes among older patients.
Google Scholar, PubMed, Scopus, CINAHL, and PsycINFO were searched using keywords like “effective communication,“ “elderly,“ and “well-being.“ Studies published between 2000 and 2023 describing or investigating communication strategies between older patients (65 years and above) and providers in various healthcare settings were considered for selection. The quality of selected studies was assessed using the GRADE Tool.
The search strategy yielded seven studies. Five studies were qualitative (two phenomenological study, one ethnography, and two grounded theory studies), one was a cross-sectional observational study, and one was an experimental study. The studies investigated the effects of verbal and nonverbal communication strategies between patients and providers on various patient-centred outcomes, such as patient satisfaction, quality of care, quality of life, and physical and mental health. All the studies reported that various verbal and non-verbal communication strategies positively impacted all patient-centred outcomes.
Although the selected studies supported the positive impact of effective communication with older adults on patient-centred outcomes, they had various methodological setbacks that need to be bridged in the future. Future studies should utilize experimental approaches, generalizable samples, and specific effect size estimates.
Peer Review reports
Introduction
Excellent communication is critical for all health professionals [ 1 , 2 ]. It affects the quality of healthcare output, impacts the patient’s health and satisfaction, and benefits both patients and providers [ 3 ]. Communication is a critical clinical competence because it establishes trust between providers and patients, creating a therapeutic relationship [ 4 ]. Physician-patient communication plays several functions, including making decisions, exchanging information, improving the physician-patient relationship, managing the patient’s doubts, addressing emotions, and enhancing self-management [ 5 ]. Features of effective or quality communication include involving patients in decisions, allowing patients to speak without interruptions, encouraging a patient to ask questions and answering the questions, using a language that the patient understands, paying attention to the patient and discussing the next steps [ 5 ]. This communication also includes listening, developing a good interpersonal relationship, and making patient-centred management plans.
The quality of patient-physician communication influences various patient-centred outcomes [ 6 ]. In this review, patient-centred outcomes refer to all the outcomes that contribute to the recovery or indicate the recovery of patients, as well as suggest positive experiences with the care process. For instance, effective communication is associated with enhanced patient satisfaction, regulating emotions, and increasing compliance, leading to improved health and better outcomes [ 7 , 8 ]. According to [ 9 ], quality communication enhances patients’ trust in their providers, making patients more satisfied with the treatment. A trusting provider-patient relationship causes individuals to believe they receive better care [ 10 ]. For instance, [ 11 ] report that effective provider-patient communication improves social, somatic, and psychological health. During communication, the provider may enhance positive motivations and involve the individual in treatment decisions. Communication helps patients to acknowledge their illnesses, the associated risks, and the advantages of consistent treatment [ 5 ]. note that mutual communication between providers and patients stimulates or strengthens patients’ perception of control over their health, the knowledge to discern symptoms and self-care and identify changes in their condition. Effective communication leads to improved perceived quality of health care [ 12 ]. report that physician-patient communication influences the perceived quality of healthcare services. All these outcomes that suggest or contribute to patient’s positive experiences or imply a positive recovery journey, such as shorter hospital stays, are considered patient-centred outcomes.
This rapid review aims to review studies that have previously investigated the influence of quality communication on patient-centred outcomes among older adults, such as psychological well-being, quality of health care, emotional well-being, cognitive well-being, individualised care, health status, patient satisfaction, and quality of life. The specific objectives include (a) exploring the strategies used to ensure quality and effective communication with older patients in various healthcare settings, (b) exploring the patient-centred health outcomes reported by previous studies investigating quality communication between providers and older patients, and (c) to link quality communication strategies with older patients to patient-centred health outcomes among older patients.
The primary rationale for conducting this rapid review is that although many studies have examined the relationship between quality communication and various patient-centred outcomes, few studies have used older patients as their participants. It is a significant research gap because older adults have unique communication needs, which, if not considered, their communication with healthcare providers could be ineffective [ 13 ]. For example, older adults experience age-related changes in cognition, perception, and sensation, which can interfere with the communication process [ 14 ]. As a result, more research is needed to the specific quality communication strategies that could improve patient-centred outcomes among older adults. To my knowledge, no systematic review has focused on this topic. Therefore, this is the first rapid review to explore quality communication and its impact on patient-centred health outcomes among older patients in various healthcare settings.
This rapid review’s findings could inform practitioners of the quality communication strategies they can use to improve patient-reported outcomes. Besides, the rapid review evaluates the quality of studies investigating this matter and makes informed recommendations for future research to advance knowledge on this subject.
This rapid review was conducted in conformity with the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines [ 15 ]. The main difference between a systematic review and a rapid review is that the former strictly conforms to the PRISMA protocol, whereas the latter can miss a few elements of a typical systematic review. A rapid review was suitable because a single reviewer was involved in the study selection process, whereas at least two independent reviewers are recommended in typical systematic reviews [ 16 ].
Eligibility criteria
Table 1 below summarises the inclusion and exclusion criteria used to guide study selection in this rapid review. Also, justification is provided for each inclusion/exclusion criteria. The inclusion/exclusion criteria were drafted based on the target population, the intervention, the outcomes, year of publication, article language, and geographical location. This approach corresponds with the PICO (P – population, I – intervention, C – comparison, and O – outcomes) framework [ 17 ].

Information sources
Four academic databases were searched: PubMed, Scopus, CINAHL, and PsycINFO. These databases were used as sources of information because they publish studies in healthcare sciences on a wide range of topics, including communication and the health outcomes of various interventions. Additionally, Google Scholar was searched to supplement the databases because it indexes academic journal articles in all disciplines, including healthcare. Combining Google Scholar with these databases has been recommended for an optimal search strategy [ 18 ].
Search strategy
Various search terms related to the critical variables of this rapid review, namely quality communication, patient-centred health outcomes, and older patients, were combined using Boolean connectors (AND & OR). Regarding quality communication, some of the keywords that were used include “quality communication,“ “effective communication,“ “doctor-patient communication,“ and “patient-centred communication.“ The keywords that were used for patient-centred outcomes included “well-being,“ “patient satisfaction,“ “quality of care,“ “health status,“ and “quality of life.“ The search terms related to older patients included “nursing home residents,“ “older,“ and “elderly.“ Additionally, since most older patients are institutionalised, search terms like “nursing homes” and “assisted living facilities” were used in the search strategy. Table 2 below presents a sample search strategy executed on PubMed between September 2022 and July 2023. As shown in Table 2 , Mesh terms were used alongside regular keywords. Truncations on the three keywords, namely elderly, nursing homes, and geriatric were used to allow more of their variations to be captured in the search. The use of Mesh terms was only performed on PubMed – Mesh terms are only supported on PubMed and MEDLINE. The rest of the sources of information were searched using the search terms without specifying whether they are Mesh terms or not.
Study selection process
One reviewer (the author) was involved in screening the studies. The reviewer screened each record at least twice for confirmation purposes. Afterwards, an automation tool called ASReview which relies on machine learning to screen textual data was used as a second confirmation [ 19 ]. Research has shown that combining a machine learning tool and a single reviewer can significantly reduce the risk of missing relevant records [ 20 ]. This decision was reached based on previous research that has also demonstrated the good sensitivity of ASReview as a study selection tool in systematic reviews [ 19 ]. The software was trained on the eligibility criteria and the broader context of this study before it was used to screen the studies and confirm the reviewer’s decision. Therefore, if a record were retrieved, the author would screen for its eligibility the first time and confirm it the second time. For the third time confirmation, ASReview was employed. In case of disagreement between the author’s first and second attempts, a third attempt could be made to resolve it. In case of disagreement between the author’s first/second/third attempts and ASReview, a fourth attempt was made to resolve it.
Data collection process
One reviewer (the author) extracted data from the qualifying records. The reviewer could collect data from a given study in the first round, record them, and confirm them in the second round. In case of disagreement between the first and second rounds, the author would extract data from the record for the third time to resolve it. The data points on which data extraction was based include the country where the study was conducted, the study’s research design (if reported), the population and setting of the study, the characteristics of the intervention (communication), and outcomes. Also, the author remained keen to identify ways the studies defined quality or effective communication in the context of older patient care. Regarding the characteristics of the intervention, some of the data sought included the type of communication (e.g., verbal or non-verbal) and the specific communicative strategies, such as touch and active listening.
Regarding outcomes, ‘patient-centred outcomes’ was used as an umbrella term for several variables that relate to the patient’s subjective well-being. Such variables include perceptions of quality of care, quality of life, symptom management, physical health, mental health, health literacy, patient satisfaction, individualised care, and overall well-being, including social processes, self-actualisation, self-esteem, life satisfaction, and psychosocial well-being. If studies reported on the acceptance and usability of communicative strategies, it was also included as a patient-centred outcome because the patient accepts a specific intervention and acknowledges its usability.
Study quality assessment
The study quality assessment in this rapid review entailed the risk of bias and certainty assessments. Risk of bias assessment formed an essential aspect of certainty assessment. The risk of bias in qualitative studies was evaluated using the Critical Appraisal Skills Program (CASP) Qualitative Checklist [ 21 ]; the Cochrane Risk of Bias (RoB) tool was used for randomised studies [ 22 ]; and Risk of Bias in Non-Randomised Studies of Interventions (ROBINS-I) was used for cross-sectional observational studies [ 23 ]. The Grading for Recommendations, Assessment, Development, and Evaluation (GRADE) tool was used to assess the certainty of the evidence for all study designs [ 24 ]. The risk of bias in each study design and its corresponding assessment tool was calculated as a percentage of the total points possible. For example, the CASP Qualitative Checklist has ten items; each awarded one point. If a study scored seven out of 10 possible points, its risk of bias would be rated as 70%. The GRADE Tool has five domains, namely risk of bias, inconsistency, indirectness, imprecision, and publication bias. The first domain, risk of bias, was populated using the findings of risk of bias assessment using the stated tools. The overall quality of a study was based upon all five domains of the GRADE Tool.
Synthesis methods
Both qualitative and quantitative studies were included in this review. The studies were highly heterogeneous in their research designs hence statistical methods like a meta-analysis synthesis were impossible [ 25 ]. Besides, the studies also had substantial heterogeneity in the study settings (some were conducted in primary care settings, but a majority were conducted in long-term care facilities/nursing homes) and outcomes. The studies measured different outcomes under the umbrella variable of patient-centred outcomes. As such, a narrative synthesis approach was considered the most suitable [ 26 ]. The narrative synthesis guidance by [ 27 ] was used. The first step based on the guidelines should be developing a theoretical model of how the interventions work, why, and for whom.
This rapid review’s explanation of how effective or quality communication leads to improved patient-centred outcomes in the introduction section formed the theoretical basis, that is, effective communication facilitates informational exchange between the patient and provider, leading to better decision-making, which positively influences patient outcomes The second step of a narrative synthesis entails organising findings from the included studies to describe patterns across the studies based on the direction of the effect size or effects [ 27 ]. The third step is to explore the relationship in the data by identifying the reasons for the direction of effects or effect size. This rapid review’s reasons were based on the theoretical notions outlined above in this paragraph. The final step is to provide insights into the generalizability of the findings to other populations, which, in the process, further research gaps can be outlined. The results are stated below.
Study selection
After running the search strategy, 40 articles were identified from PubMed, 13 from Google Scholar (records identified from websites (Fig. 1 )), 24 from Scopus, 18 from CINHAL, and 10 from PsycINFO based on the relevance of the titles. It was discovered that 26 were duplicated records between databases and Google Scholar, which reduced the number of identified records to 79. Further, the automation tool (ASReview) marked five records as ineligible based on their title considering the inclusion and exclusion criteria. These articles were excluded because the author confirmed in the fourth round that they were ineligible. After realising they did not focus on older adults, the author excluded three more records. Therefore, 71 records were screened using their abstracts with the help of ASReview (64 records from databases and 7 records from Google Scholar), whereby 44 were excluded (40 records from databases and 4 records from Google Scholar) for various reasons, such as being expert opinions and professional development based on field experiences (e.g., [ 28 ]) and did not have a methodology. The remaining 27 records (24 records from databases and 3 records from Google Scholar) were sought for retrieval, whereby one was excluded because its full text was inaccessible. The remaining 26 articles (23 records from databases and 3 records from Google Scholar) were assessed for eligibility with the help of ASReview, whereby eight records were excluded because they did not report their methodologies (e.g., [ 29 ]), another eight were secondary studies (e.g., [ 30 ]), and three were non-peer-reviewed preprints. Therefore, seven studies met the eligibility criteria for this rapid review.
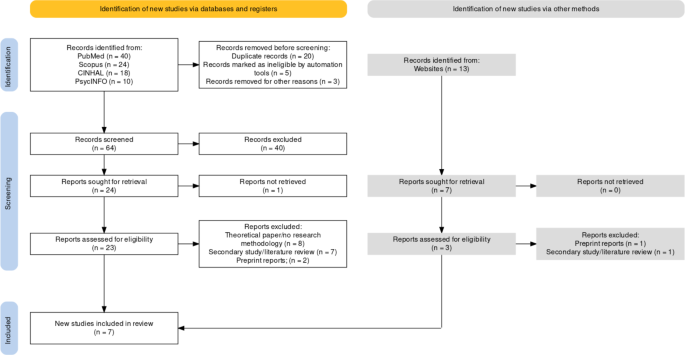
PRISMA Flowchart summarising the study selection process
Study characteristics
Out of the seven studies, one was an experimental study [ 31 ], one was a cross-sectional observational study [ 32 ], and five were qualitative studies [ 33 , 34 , 35 , 36 , 37 ]. As shown in Table 3 , most of the studies (n = 4) were conducted in the United States. The following countries produced one study each: Australia, Cameroon, the Netherlands, and Hungary. Although all the studies utilised a sample of older patients, the characteristics of the patients differed from one study to another. The studies ranged from primary care settings [ 36 ] and adult medical wards [ 37 ] to long-term care facilities like nursing homes. Apart from [ 36 ], the rest of the studies investigated various non-verbal communication strategies with older adults and their impact on various types of patient-centred outcomes, ranging from health-related outcomes (e.g., smoking cessation) to patient-reported outcomes, such as patient satisfaction, self-esteem, and life satisfaction. These outcomes are within the broader umbrella category of patient-centred m outcomes.
Further, the studies used different types of communicative strategies that can be used to enhance or promote patient-centred outcomes. In this rapid review, they were categorised into seven, namely (a) touching, (b) smiling, (c) gaze, head nod, and eyebrow movement, (d) active listening, (e) close physical distance, and (f) use of visual aids, and (g) telephone communication. Table 4 summarises the various ways in which each study described its interventions.
Quality assessment findings
All seven studies were of high quality based on the GRADE Tool-based Assessment. However, [ 31 ] conducted an experimental study, but they did not provide any details indicating whether there was concealment in participant allocation and blinding of participants and outcome assessors. Therefore, it has a high likelihood of risk of bias. However, they scored excellently in the other domains of the GRADE Tool. All five qualitative studies and the cross-sectional observational study also scored excellently in the domains of the GRADE Tool, apart from the imprecision domain where they could not be scored because none of them reported effect sizes (Table 5 ).
Results of individual studies
[ 31 ] was the only experimental study used in this rapid review investigating the effect of comfort touch on older patients’ perceptions of well-being, self-esteem, health status, social processes, life satisfaction, self-actualisation, and self-responsibility. The authors did not report the effect sizes but indicated that comforting touch had a statistically significant effect on each of the five variables. In summary, the authors suggested that comfort touch, characterised by a handshake or a pat on the shoulders, forearm, or hand, had a statistically significant positive impact on the various patient-centred outcomes reported in their study. For each variable, the authors used three groups, the first and second control groups and the third experimental group. After delivering the intervention, they investigated whether the scores of these variables changed between three-time points in each of the three groups. The first time point was the baseline data collected before intervention was initiated; the second was two weeks after baseline data; and the third was four weeks after baseline data. The authors found that in each of the five variables, the scores remained almost the same in the three-time points for the two control groups, but there were significant improvements in the experimental group (the one that received the intervention). For example, the self-esteem variable was measured using Rosenberg’s Self-Esteem Scale, with the highest attainable score of 40. In the first control group, the score remained 27.00, 27.27, and 27.13 for Time 1 (baseline), Time 2 (after two weeks), and Time 3 (after four weeks), respectively. The same trend was observed in the second control group. However, in the experimental group, the score improved from 29.17 at baseline to 36.00 at Time 2 and 37.47 at Time 3. These findings suggest that comfort touch was highly effective in improving self-esteem among older patients. The same significant improvements were evident for all the other variables (p.184).
While all the other studies focused on nonverbal communication cues, [ 36 ] focused on telephone communication. They aimed to investigate the effect of a tailored intervention on health behaviour change in older adults delivered through telephone communication. Therefore, the primary rationale for selecting this study for review is that it used a specific communicative strategy (telephone) to deliver the intervention, which is the primary purpose of effective communication in most healthcare settings. The older patients used as participants in this study lived with COPD. The nurses trained to administer the intervention made regular phone calls over 12 months. The intervention was delivered to 90 participants. Of these, 65 were invited for interviews at the end of 12 months. One of the most important outcomes relevant to this rapid review is that the participants reported “being listened to by a caring health professional.“ It means that regular telephone communication improved the patient’s perceptions of the quality of care. Other critical patient-centred outcomes that improved due to this intervention include many participants quitting smoking and increased awareness of COPD effects.
[ 34 ] also conducted a qualitative study but needed to specify the specific research design, which was generally non-experimental. The authors used formative evaluation and a participatory approach to develop a communicative intervention for older adults with limited health literacy. In other words, apart from literature reviews, the authors involved the target population in developing a curated story to improve their health literacy. They developed photo and video-based stories by incorporating narrative and social learning theories. The most important finding of this study was that the authors found the developed communicative strategy appealing and understandable. Such observations imply that the participants’ health literacy also likely improved even though the authors did not evaluate it.
Further, using a sample of 155 older patients, [ 32 ] investigated the relationship between the communication characteristics between nursing practitioners and the older patients and patients’ proximal outcomes, namely patient satisfaction and intention to adhere to the NPs’ recommendations, and patients’ long-term outcomes (presenting problems and physical and mental health). The proximal outcomes (satisfaction and intention to adhere) were measured after visits, whereas the long-term outcomes (presenting problems, mental health, and physical health) were measured at four weeks. The communication and relationship components observed include various non-verbal communication strategies: smile, gaze, touch, eyebrow movement, head nod, and handshakes. The authors recorded videos during patient-provider interactions. These communicative strategies were measured using the Roter Interaction Analysis System (independent variable).
In contrast, the other outcomes (dependent variables) outlined above were each measured separately with a validated tool or single-item instruments [ 32 ]. For example, presenting problems were measured with a single-item instrument, whereas the physical and mental health changes at four weeks were measured using the SF-12 Version 2 Health Survey. The authors found that verbal and nonverbal communication strategies focused on providing patients with biomedical and psychosocial information and positive talk characterised by receptivity and trust were associated with better patient outcomes, such as significant improvements in mental and physical health at four weeks. Although the study did not report effect sizes, the findings agree that effective and quality communication can improve patient-centred outcomes like patient satisfaction.
[ 35 ] conducted a qualitative study with focus groups (eight focus groups with a range of three to nine participants) of 15 older adults in a nursing home. The study used an ethnographic qualitative design. The nonverbal communication strategies observed in this study included active listening (including verbal responses) and touching. The authors found that the characteristics of the communication strategies that make communication quality and effective include mutual respect, equity, and addressing conflict. The patients perceived that their nursing aides gave them better-individualised care if their relationship and communication were characterised by mutual respect. Portraying mutual respect includes showing the patients that they are being listened to and heard, which can include calling them by their names and showing signs of active listening. Some residents (older patients) complained that some nursing aides had favouritism, whereby they liked some patients and not others. When such a perception emerges, the patients could perceive the treatment as unjust, compromising individualised care quality. Also, nursing aides must equip themselves with communicative strategies to address conflict rather than avoid it. For example, knowing about the patient’s history can help nursing aides understand their behaviour in the facility, improving prospects of providing better personalised or individualised care.
[ 33 ] also conducted a qualitative study utilising a sample of 17 older adults in nursing homes and assisted living facilities in the United States. They aimed to identify the types and examples of nurse-aide-initiated communication with long-term care residents during mealtime assistance in the context of the residents’ responses. Using a naturalistic approach, the researchers observed communicative interactions between the nurse aides and the residents during mealtime assistance. Videos were recorded and transcribed and analysed using the grounded theory approach. They found that apart from emotional support, nonverbal communication strategies were used by nurse aides to address the residents, initiate and maintain personal conversations, and check-in. Although the authors did not provide statistical proof that these communication strategies improved well-being, their findings can inform future studies.
Finally, [ 37 ] conducted a qualitative, grounded theory study to develop a model for effective non-verbal communication between nurses and older patients. The authors conducted overt observations of patient-nurse interactions using a sample of eight older patients. They found that the nature of nonverbal communication to be employed depends on the context or environment, and certain external factors influence it. The factors influencing nonverbal communication include the nurses’ intrinsic factors, positive views of older adults, awareness of nonverbal communication, and possession of nonverbal communication skills. Patient factors that can also influence the effectiveness of nonverbal communication include positive moods, financial situations, and non-critical medical conditions. The model developed also emphasised that non-verbal communication, if carried out correctly considering context and environment, can lead to positive outcomes, such as increased adherence to providers’ recommendations, improved quality of care, and shorter hospital stays.
Results of syntheses
Four themes emerged from the narrative synthesis: nonverbal communication, verbal communication, communication strategies, and patient-centred outcomes. Table 6 summarises the subthemes that emerged under each theme. They are discussed below.
Nonverbal communication
Nonverbal communication was a critical theme that emerged in several studies. Five out of the seven studies investigated the effectiveness of touch on various patient-centred outcomes [ 31 ]. found that nonverbal communication strategies such as comfort touch, characterised by a handshake or a pat on the shoulders, forearm, or hand, had a statistically significant positive impact on patient-centred outcomes, such as well-being, self-esteem, health status, social processes, life satisfaction, self-actualisation, and self-responsibility [ 31 ]. implemented comfort touch exclusively without combining it with other nonverbal communication strategies. It means that comfort touch on its own can be effective in improving various patient-centred outcomes. As such, it can be hypothesised that if comfort touch is combined with other nonverbal communication strategies, such as active listening, eye gazing, smiling, maintaining a close distance, eyebrow movement, and nodding/shaking of the head can lead to even better results regarding patient-centred outcomes [ 32 , 33 , 35 , 37 ]. [ 35 ] identified active listening and touching as important nonverbal communication strategies that make communication quality and effective [ 33 ]. found that nurse-aide-initiated communication during mealtime assistance using nonverbal communication strategies, such as emotional support, smiling, laughing, touching, eye gazing, shaking hands, head nodding, leaning forward, and a soft tone were crucial in addressing the residents, initiating (and maintaining) personal conversations, and checking in. Finally, [ 37 ] developed a model that emphasised the importance of effective nonverbal communication in forming effective therapeutic relationships, promoting patient satisfaction, and improving the quality of care. An exhaustive list of the nonverbal communication approaches is shown in Table 6 .
In general, most studies, especially the qualitative ones, supported the utilisation of multiple non-verbal communication strategies in a single communicative episode. The studies also implied that it is the responsibility of healthcare providers to initiate and maintain effective nonverbal communication cues, such as those detailed in Table 6 . Additionally, it is important to note that it is only one study [ 31 ] that investigated the effectiveness of comfort touch on patient-centred outcomes. Therefore, the notion implied in qualitative studies that combining various nonverbal strategies could lead to a better improvement in patient-centred outcomes is subject to further empirical investigation. It was noted that there is a lack of empirical studies investigating how the combination of various non-verbal communication techniques or strategies can influence patient-centred outcomes, such as patient satisfaction and perceptions of quality of care.
Verbal communication
Four out of the seven studies implied that verbal communication improved patient-centred outcomes [ 32 , 34 , 35 , 36 ]. Effective and quality verbal communication was found to impact patient satisfaction positively [ 32 ], increased awareness of COPD effects [ 36 ], improved health literacy [ 34 ], presented problems [ 32 ], and mental and physical health [ 32 ]. It is worth noting that [ 32 ] used a cross-sectional survey approach and used regression analyses to investigate the relationship between communication and various patient-centred outcomes, such as patient satisfaction and mental and physical health. Also, it is important noting that the authors combined both verbal (e.g., more positive talk, greater trust, and receptivity) and non-verbal (e.g., smile, gazing, eyebrow movements, and interpersonal touches) in their study. Therefore, it can be a bit challenging to directly conclude that effective verbal communication alone without non-verbal communication is effective on its own in improving patient-centred outcomes. Similarly, [ 34 ] combined both narrative-based and picture-based communication strategies to give patients education about health literacy. Therefore, it can be challenging to know whether narratives comprising of verbal communication (and often non-verbal communication) can improve patient-centred outcomes on their own. The rest of the studies were qualitative [ 35 , 36 ], which means that their findings generally reflected the subjective experiences or opinions of their participants. Therefore, it can be said that although all the four studies supported verbal communication can effectively improve patient-centred outcomes, there is a need for future research to experimentally test its effectiveness without being combined with non-verbal communication strategies.
Moreover, two of the four studies implied that some conditions must be met for verbal communication to be effective [ 32 , 35 ]. some communication strategies, such as higher lifestyle discussion and rapport-building rates, were perceived as patronising and associated with poor outcomes [ 32 ]. Instead, the authors found that communication strategies like seeking and giving biomedical and psychosocial information were more effective in improving patient outcomes [ 32 ]. It implies that healthcare providers should be attentive and intentional of the topics they discuss with patients. Further, in their qualitative study, [ 35 ] found that effective verbal communication also requires mutual respect, equity, and addressing conflict. Indeed, it appears that certain communication strategies like lifestyle discussions can undermine the process of establishing trust, which is why they were associated with adverse patient outcomes. Also, unlike nonverbal communication, the studies that highlighted the effect of verbal communication on patient-centred outcomes did not provide rich descriptions of the specific verbal communication strategies that can be used in a face-to-face healthcare setting. The described strategies like using phone calls to regularly communicate with the patient without having to visit a healthcare facility and things to ensure when communicating with the older patient, such as mutual respect and avoiding too many discussions on lifestyle do not offer rich insights into the specific nature of the verbal communication strategies.
Communication strategies
In 3.5.2 above, it was shown that the sample of participants that [ 32 ] used in their study did not prefer discussions related with healthy lifestyles, which compromised patient-centred outcomes. Therefore, it was also important to determine the best approaches to formulate communication strategies that work. Two out of the seven studies implied how communication strategies can be formulated [ 34 , 36 ] [ 36 ]. found that a tailored intervention delivered through telephone communication improved patient perceptions of the quality of care. In this regard, the authors first identified the needs of the patients to guide the development of the tailored intervention, from which they might have obtained insights into the patients’ communication preferences [ 34 ]. found a participatory approach to developing a curated story that improves health literacy appealing and understandable. The findings emphasised the need for participatory approaches when developing communication interventions for patients with varied health and social needs. Although the studies did not compare or contrast the effectiveness of participatory-based communication strategies and non-participatory-based communication strategies, their findings provide useful insights into the significance of involving patients when developing them. From their findings, it can be anticipated that a participatory approach is more likely to yield better patient-centred outcomes than non-participatory-based communication strategies.
Patient-centred outcomes
All studies reviewed highlighted patient-centred outcomes as the goal of effective communication in older patients. Patient-centred outcomes included well-being, self-esteem, health status, social processes, life satisfaction, self-actualisation, and self-responsibility (Butt, 2001), as well as patient satisfaction [ 32 , 36 ], increased awareness of COPD effects [ 36 ], and improved health literacy [ 34 ]. Others included presenting problems, mental health, and physical health [ 32 ], as well as adherence to providers’ recommendations, improved quality of care, and shorter hospital stays [ 37 ]. All seven studies indicated that the various verbal and nonverbal communication approaches could improve these patient-centred outcomes. The consistency observed between the experimental study by [ 31 ], the qualitative studies, and other quantitative study designs implies the need to pay greater attention to verbal and non-verbal communication strategies used by healthcare professionals as they can directly influence numerous patient-centred outcomes. This consistency further implies that effective communication is the anchor of high-quality care, and its absence will always compromise patient-centred outcomes, such as satisfaction and health outcomes.
Discussion and conclusion
Discussion of findings.
In agreement with various studies and reviews conducted in younger populations [ 1 , 2 , 3 ], all the seven studies selected in this rapid review supported that effective communication is a cornerstone of improved patient-centred outcomes. Like [ 5 , 11 , 12 ], the studies reviewed in this rapid review also supported the idea that effective communication with older adults involves the combination of verbal and nonverbal communication cues. However, this rapid review went a step ahead to identify the specific conditions that must be present for effective verbal and nonverbal communication to take place, such as perceptions of equity, mutual respect, and addressing conflict instead of avoiding it. The qualitative studies used in this rapid review also offered rich descriptions of how providers use nonverbal communication strategies.
However, the main shortcoming of the seven studies reviewed is that none aimed to define or describe what constitutes effective communication with older adults, apart from [ 37 ], who described a model of nonverbal communication with older adults. The study was qualitative and only formed a theoretical basis of how effective nonverbal communication with older adults could be shaped. The theory developed needs to be tested in an experimental setting so that its effect size in improving patient-centred outcomes, such as quality of care, quality of life, patient satisfaction, and emotional and cognitive well-being, can be documented unbiasedly and validly. Therefore, as much as the reviewed studies agreed with younger populations regarding the positive effect of effective and quality communication on patient-centred outcomes [ 9 , 10 ], the methodological rigour of studies with older patients needs to be improved.
Although the individual studies reviewed in this rapid review had low risk of bias apart from [ 31 ], the screening was based on the judgment of the individual research designs. Otherwise, if the assessment had been done from the perspective of the focus of this rapid review, the risk of bias in studies could have been high in predicting the influence of effective communication on patient-centred outcomes. First, apart from [ 31 ], none of the studies used a random sample. The qualitative studies used purposively obtained samples, which means the risk of bias from an interventional perspective was high. However, the studies provided in-depth insights into the characteristics and features of verbal and non-verbal communication strategies that can be used to form and maintain provider-patient relationships.
Recommendations for practice and future research
The main recommendation for practice is that nurses and providers serving older patients must be aware of their verbal and non-verbal communication strategies. Besides, they should engage in continuous professional development to enhance their verbal and non-verbal communication skills. Combining a wide range of nonverbal communication, such as touching the patient on the shoulder or arm or even handshaking can help create strong bonds and relationships, which are key in an effective therapeutic relationship. The qualitative studies reviewed showed that nurses and other providers combine a wide range of nonverbal communication in a single interaction instance, such as eye gazing, nodding, touching, and eyebrow movement. Although studies on verbal communication were rare in this rapid review, some lessons learned from the few studies included (e.g., [ 36 ]) is that using telephones to communicate with older patients regularly is potentially effective in improving patient-centred outcomes like better self-management. The information shared by the nurse should be tailored to serve the specific health needs of older patients. For example, for COPD patients, a nurse can make regular calls to old patients to educate them about the importance of quitting smoking and alcohol to improve their health condition and better self-management. However, as [ 32 ] indicated, the nurse should be cautious about how to present the information to the client and be able to detect patronising discussions quickly. For example, the sample of adults used by [ 32 ] found that many lifestyle and rapport-building discussions with the nurse were patronising in ways that may be detrimental to patient-centred outcomes. Some of the strategies providers can employ to ensure that communication is not perceived as patronising by older patients include ensuring mutual respect (e.g., active listening as a sign of mutual respect), creating perceptions of equity rather than favouritism when communicating with multiple patients at a time, and solving conflicts rather than avoiding them, which entails extra efforts, such as understanding the patient’s behaviour in the past and present. Overall, although studies have not provided specific estimates of the effect sizes of effective communication on patient-centred outcomes among older adults, there is a general trend and consensus in studies that effective communication, nonverbal and verbal, is the cornerstone of high-quality healthcare.
Further, future research needs to address various gaps identified in this study. The first gap is that although [ 37 ] tried to develop a model of nonverbal communication with older adults, their study had some drawbacks that limited the comprehensiveness of the model. First, the authors used a sample of only eight older adults in two medical wards in Cameroon. Besides the small sample, the study was conducted in medical wards, which means its findings may not be generalisable to long-term care settings like nursing homes. More older adults who encounter healthcare professionals are admitted in long-term care facilities, calling for developing a more robust communication strategy. Second, [ 37 ] only focused on nonverbal communication, thereby providing limited practical applicability of the model since verbal and nonverbal communication co-exists in a single interactional instance. Therefore, there is a need to develop a model that provides a complete picture into what effective communication is like with older adults.
After developing a valid, reliable, and generalisable model for effective communication with older adults in various healthcare settings, future research should also focus on investigating the impact of such a model on patient-centred outcomes, such as quality of care, quality of life, patient satisfaction, and physical and mental health. More particularly, the developed model can be used to derive communication interventions, which can be applied and tested in various healthcare settings with older adults. That way, research on this subject matter will mature as more and more studies test the effectiveness of such a communication model in various settings and countries. All that is known in the literature is that effective verbal and nonverbal communication can help promote patient-centred outcomes among older adults.
Limitations
Although this rapid review was conducted rigorously by adhering to the PRISMA guidelines, the use of a single reviewer in the study selection process can undermine the quality of the review. When a single reviewer is involved, the probability of missing out relevant studies increases immensely. However, this limitation was mitigated in this review by using an automation tool in the study selection process. In was assumed that combining the automation tool with one independent reviewer could significantly reduce the probability of missing relevant studies.
Another possible limitation is that few studies have been conducted between 2000 and 2023 investigating the effect of effective communication on various patient-centred outcomes. Although the literature recognises the importance of effective communication, and there is a unanimous agreement between studies of various research designs that it is the cornerstone of quality of care, more studies need to be conducted examining how various communication strategies influence patient outcomes, both subjective and objective. For example, [ 31 ] investigated the effect of comfort touch. Other studies using empirical means (e.g., experiments) can also test the other strategies identified, such as eye gazing, head nodding, eyebrow movement, et cetera. In this way, a more specific and structured approach to communication in healthcare settings can be developed using the evidence base.
Moreover, I initially intended to review studies published within the past five years (2018–2023) but later learned there were insufficient studies meeting the eligibility criteria. Consequently, I adjusted the publication date to the past ten years (2013–2023). I also learned insufficient studies published within that period. Consequently, I chose the period of 2000–2023, which yielded seven studies. Thus, some of the studies included may not capture contemporary realities in healthcare settings, raising the need for more empirical studies on this topic.
This rapid review selected seven studies whose narrative synthesis demonstrated that effective verbal and non-verbal communication could improve patient-centred outcomes. However, the studies were mostly qualitative, and hence they only provided rich descriptions of how nurses and older patients communicate in various clinical settings. It is only one study (Butts, 2001) that was experimental. Still, its risk of bias was high since patients were not concealed to allocation, and participants and outcome assessors were not blinded. Future research needs to focus on deriving a valid, reliable, and generalisable communication model with older adults using a larger and more representative sample size of older patients. Such a model should encompass both verbal and nonverbal communication. After developing a robust model, the next phase of future studies is to derive interventions based on the model and then, through experimental research, test their effectiveness. In that way, a standard approach to communicating effectively and in quality will be achieved, which is yet to be achieved in the current studies.
Data Availability
All data generated or analysed during this study are included in this published article [and its supplementary information files].
Alnaser F. Effective communication skills and patient’s health. CPQ Neurol Psychol. 2020;3(4):1–11.
Google Scholar
Skarbalienė A, Skarbalius E, Gedrime L. Effective communication in the healthcare settings: are the graduates ready for it? Management (Split, Online). 2019;24:137–47.
Holm A, Karlsson V, Dreyer P. Nurses’ experiences of serving as a communication guide and supporting the implementation of a communication intervention in the intensive care unit. Int J Qualitative Stud Health Well-being. 2021;16(1):1971598.
Article Google Scholar
Chichirez CM, Purcărea VL. Interpersonal communication in healthcare. J Med Life. 2018;11(2):119–22.
CAS PubMed PubMed Central Google Scholar
Świątoniowska-Lonc N, Polański J, Tański W, Jankowska-Polańska B. Impact of satisfaction with physician–patient communication on self-care and adherence in patients with hypertension: cross-sectional study. BMC Health Serv Res. 2020;20(1):1046.
Article PubMed PubMed Central Google Scholar
Cuffy C, Hagiwara N, Vrana S, McInnes BT. Measuring the quality of patient–physician communication. J Biomed Inform. 2020;112:103589.
Ghosh AK, Joshi S, Ghosh A. Effective patient-physician communication - A concise review. J Assoc Physicians India. 2020;68(6):53–7.
PubMed Google Scholar
Surbakti F, Sari K. The relationship between consultation length and patient satisfaction: a systematic review. KLS. 2018;4(9):41.
Birkhäuer J, Gaab J, Kossowsky J, Hasler S, Krummenacher P, Werner C, et al. Trust in the health care professional and health outcome: a meta-analysis. Nater UM. editor PLoS ONE. 2017;12(2):e0170988.
Chandra S, Ward P, Mohammadnezhad M. Factors associated with patient satisfaction in outpatient department of Suva Sub-divisional Health Center, Fiji, 2018: a mixed method study. Front Public Health. 2019;7:183.
Choi E, Chentsova-Dutton Y, Parrott WG. The effectiveness of somatization in communicating distress in Korean and American cultural contexts. Front Psychol [Internet]. 2016 Mar 23 [cited 2023 Mar 16];7. Available from: http://journal.frontiersin.org/Article/ https://doi.org/10.3389/fpsyg.2016.00383/abstract .
Chandra S, Mohammadnezhad M, Ward P. Trust and communication in a doctor- patient relationship: A literature review. J Healthc Commun [Internet]. 2018 [cited 2023 Mar 16];03(03). Available from: http://healthcare-communications.imedpub.com/trust-and-communication-in-a-doctorpatient-relationship-a-literature-review.php?aid=23072 .
Wanko Keutchafo EL, Kerr J, Jarvis MA. Evidence of nonverbal communication between nurses and older adults: a scoping review. BMC Nurs. 2020;19(1):53.
Brooks C, Ballinger C, Nutbeam D, Adams J. The importance of building trust and tailoring interactions when meeting older adults’ health literacy needs. Disabil Rehabil. 2017;39(23):2428–35.
Article PubMed Google Scholar
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;n71.
Waffenschmidt S, Knelangen M, Sieben W, Bühn S, Pieper D. Single screening versus conventional double screening for study selection in systematic reviews: a methodological systematic review. BMC Med Res Methodol. 2019;19(1):132.
Kloda LA, Boruff JT, Soares Cavalcante A. A comparison of patient, intervention, comparison, outcome (PICO) to a new, alternative clinical question framework for search skills, search results, and self-efficacy: a randomized controlled trial. jmla [Internet]. 2020 Apr 1 [cited 2023 Jan 3];108(2). Available from: http://jmla.pitt.edu/ojs/jmla/article/view/739 .
Bramer WM, De Jonge GB, Rethlefsen ML, Mast F, Kleijnen J. A systematic approach to searching: an efficient and complete method to develop literature searches. jmla [Internet]. 2018 Oct 4 [cited 2023 Jan 3];106(4). Available from: http://jmla.pitt.edu/ojs/jmla/article/view/283 .
van de Schoot R, de Bruin J, Schram R, Zahedi P, de Boer J, Weijdema F, et al. An open source machine learning framework for efficient and transparent systematic reviews. Nat Mach Intell. 2021;3(2):125–33.
Gates A, Guitard S, Pillay J, Elliott SA, Dyson MP, Newton AS, et al. Performance and usability of machine learning for screening in systematic reviews: a comparative evaluation of three tools. Syst Rev. 2019;8(1):278.
Long HA, French DP, Brooks JM. Optimising the value of the critical appraisal skills programme (CASP) tool for quality appraisal in qualitative evidence synthesis. Res Methods Med Health Sci. 2020;1(1):31–42.
Higgins JP, Savović J, Page MJ, Elbers RG, Sterne JA et al. Assessing risk of bias in a randomized trial. In: Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, editors. Cochrane Handbook for Systematic Reviews of Interventions [Internet]. 1st ed. Wiley; 2019 [cited 2023 Feb 15]. p. 205–28. Available from: https://doi.org/10.1002/9781119536604.ch8 .
Sterne JA, Hernán MA, McAleenan A, Reeves BC, Higgins JP et al. Assessing risk of bias in a non-randomized study. In: Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, editors. Cochrane Handbook for Systematic Reviews of Interventions [Internet]. 1st ed. Wiley; 2019 [cited 2023 Mar 16]. p. 621–41. Available from: https://doi.org/10.1002/9781119536604.ch25 .
Zhang Y, Alonso-Coello P, Guyatt GH, Yepes-Nuñez JJ, Akl EA, Hazlewood G, et al. GRADE guidelines: 19. Assessing the certainty of evidence in the importance of outcomes or values and preferences—risk of bias and indirectness. J Clin Epidemiol. 2019;111:94–104.
Al khalaf MM, Thalib L, Doi SAR. Combining heterogenous studies using the random-effects model is a mistake and leads to inconclusive meta-analyses. J Clin Epidemiol. 2011;64(2):119–23.
Campbell M, Thomson H, Katikireddi SV, Sowden A. Reporting of narrative synthesis in systematic reviews of public health interventions: a methodological assessment. The Lancet. 2016;388:34.
Popay J, Roberts H, Sowden A, Petticrew M, Arai L, Rodgers M et al. Guidance on the conduct of narrative synthesis in systematic reviews: A product from the ESRC Methods Programme [Internet]. Lancaster University; 2006 [cited 2023 Mar 16]. Available from: https://doi.org/10.13140/2.1.1018.4643 .
Daly L. Effective communication with older adults. Nurs Standard. 2017;31(41):55–63.
Calcagno KM. Listen up ??? Someone important is talking. Home Healthc Nurse: J Home Care Hospice Prof. 2008;26(6):333–6.
Williams K. Evidence-based strategies for communicating with older adults in long-term care. J Clin Outcomes Manage. 2013;20(11):507–12.
Butts JB. Outcomes of comfort touch in institutionalized elderly female residents. Geriatr Nurs. 2001;22(4):180–4.
Article CAS PubMed Google Scholar
Gilbert DA, Hayes E. Communication and outcomes of visits between older patients and nurse practitioners. Nurs Res. 2009;58(4):283–93.
Carpiac-Claver ML, Levy-Storms L. In a manner of speaking: communication between nurse aides and older adults in long-term care settings. Health Commun. 2007;22(1):59–67.
van ’t Jagt K, de Winter R, Reijneveld AF, Hoeks SA, Jansen JCJ. Development of a communication intervention for older adults with limited health literacy: photo stories to support doctor–patient communication. J Health Communication. 2016;21(sup2):69–82.
Levy-Storms L, Claver M, Gutierrez VF, Curry L. Individualized care in practice: communication strategies of nursing aides and residents in nursing homes. J Appl Communication Res. 2011;39(3):271–89.
Walters JAE, Cameron-Tucker H, Courtney-Pratt H, Nelson M, Robinson A, Scott J, et al. Supporting health behaviour change in chronic obstructive pulmonary disease with telephone health-mentoring: insights from a qualitative study. BMC Fam Pract. 2012;13(1):55.
Wanko Keutchafo EL, Kerr J, Baloyi OB. A model for effective nonverbal communication between nurses and older patients: a grounded theory inquiry. Healthcare. 2022;10(11):2119.
Download references
Acknowledgements
I thank my wife and children for their patience and the great opportunity to devote a lot of time to doing the article in the best possible way.
Author information
Authors and affiliations.
Faculty of Graduate Studies, Arab American University, 13 Zababdeh, P.O Box 240, Jenin, Palestine
Samer H. Sharkiya
You can also search for this author in PubMed Google Scholar
Contributions
I am the primary and sole author of this article. My contribution to this article is a full contribution.
Corresponding author
Correspondence to Samer H. Sharkiya .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Ethics approval and consent to participate
‘Not applicable’ for that section. The article is a rapid review type.
Consent for publication
Not applicable.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Sharkiya, S.H. Quality communication can improve patient-centred health outcomes among older patients: a rapid review. BMC Health Serv Res 23 , 886 (2023). https://doi.org/10.1186/s12913-023-09869-8
Download citation
Received : 07 April 2023
Accepted : 01 August 2023
Published : 22 August 2023
DOI : https://doi.org/10.1186/s12913-023-09869-8
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Effective communication
- Patient outcomes
BMC Health Services Research
ISSN: 1472-6963
- General enquiries: [email protected]

IMAGES
VIDEO
COMMENTS
Background The growing adoption of continuous quality improvement (CQI) initiatives in healthcare has generated a surge in research interest to gain a deeper understanding of CQI. However, comprehensive evidence regarding the diverse facets of CQI in healthcare has been limited. Our review sought to comprehensively grasp the conceptualization and principles of CQI, explore existing models and ...
Improving the quality of health care across a nation is complex and hard. Countries often rely on multiple single national level programmes to make progress. ... She originally trained in medicine, is a specialist in public health and health policy research, and has published widely. Acknowledgements. none. Author's contributions. The author ...
Background: Evidence-based practice and decision-making have been consistently linked to improved quality of care, patient safety, and many positive clinical outcomes in isolated reports throughout the literature. However, a comprehensive summary and review of the extent and type of evidence-based practices (EBPs) and their associated outcomes across clinical settings are lacking.
One of the most widely accepted classifications of health care quality was developed by the US National Academy of Medicine. [2] It defines six pillars of high-quality care: safety, effectiveness, patient-centeredness, timeliness, efficiency, and equity (see Table 1).Despite this apparent consensus, in practice these domains are considered unevenly.
Exploring the actionability of healthcare performance indicators for quality of care: a qualitative analysis of the literature, expert opinion and user experience. BMJ Quality & Safety 2021;30:1010-20. [PMC free article] 18. Nolte E. International benchmarking of healthcare quality: a review of the literature.
Moreover, research 8 - 11 has shown that the health-care system is facing a myriad of challenges which include high care cost, swiftly increasing dependence on technology, economic pressure on health organizations, reduction in health-care quality, 8, 10 fulfillment of patients' needs, 9 augmented numbers of patients who are suffering from ...
Quality of care is the extent to which the health care system can achieve the desired health care goals, such as effective recovery, preventing premature mortality, halting disease progression from being complicated, and maximising clients' satisfaction with the care they received [].With efficient, integrated, equitable, timely, people-centred, and safe health services, preventive and ...
The field of quality measurement in healthcare has developed considerably in the past few decades and has attracted growing interest among researchers, policy-makers and the general public (Papanicolas & Smith, 2013; EC, 2016; OECD, 2019). Researchers and policy-makers are increasingly seeking to develop more systematic ways of measuring and benchmarking quality of care of different providers.
Health system quality has received much attention since The Lancet Global Health Commission on high quality health systems in 2018, which proposed new ways to define, measure, and improve the performance of health systems.1 Factors influencing quality of health systems are well known, both as inputs and processes, including WHO's six building blocks (service delivery, health workforce, health ...
Background Effective communication is a cornerstone of quality healthcare. Communication helps providers bond with patients, forming therapeutic relationships that benefit patient-centred outcomes. The information exchanged between the provider and patient can help in medical decision-making, such as better self-management. This rapid review investigated the effects of quality and effective ...